カルシフェジオール
Calcifediol/ja
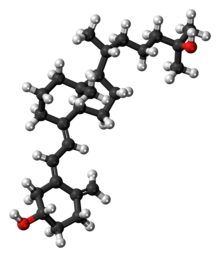
カルシフェジオール(Calcifediol)は、カルシジオール、25-ヒドロキシコレカルシフェロール、または25-ヒドロキシビタミンD3(略称25(OH)D3)としても知られている、 は、ビタミンD3(コレカルシフェロール)が酵素ビタミンD 25-水酸化酵素によって肝臓で水酸化されることによって生成されるビタミンDの一種である。カルシフェジオールは酵素によってさらに水酸化される。主に腎臓に存在する25(OH)D-1α-ヒドロキシラーゼによってさらに水酸化され、活性型ビタミンDであるカルシトリオール(1,25-(OH)2D3)となる。

| |
| |
| Names | |
|---|---|
| Preferred IUPAC name
(1S,3Z)-3-[(2E)-2-{(1R,3aS,7aR)-1-[(2R)-6-Hydroxy-6-methylheptan-2-yl]-7a-methyloctahydro-4H-inden-4-ylidene}ethylidene]-4-methylidenecyclohexan-1-ol | |
| Other names
25-Hydroxyvitamin D3
25-Hydroxycholecalciferol Calcidiol | |
| Identifiers | |
3D model (JSmol)
|
|
| ChEBI | |
| ChEMBL | |
| ChemSpider | |
| DrugBank | |
| KEGG | |
| MeSH | Calcifediol |
PubChem CID
|
|
| UNII | |
| |
| |
| Properties | |
| C27H44O2 | |
| Molar mass | 400.64 g/mol |
| Pharmacology | |
| H05BX05 (WHO) | |
カルシフェジオールは血液中でビタミンD結合タンパク質と強く結合している。血清カルシフェジオールの測定は、ビタミンD欠乏または充足を示すために、人のビタミンDの状態を決定するために行われる通常の検査である。カルシフェジオールは、ビタミンDを補充する経口医薬品として一部の国で販売されている。
生化学
カルシフェジオールは、活性型ビタミンDであるカルシトリオールの前駆体であり、肝臓でコレカルシフェロール(ビタミンD3)の25位を水酸化することにより合成される。この酵素的な25位水酸化酵素反応は、ミクロソームに存在するCYP2R1の作用によるところが大きいが、ミトコンドリアCYP27A1などの他の酵素が寄与することもある。肥満における低レベルなど、CYP2R1の発現および活性の変動は、循環カルシフェジオールに影響を及ぼす。同様に、ビタミンD2であるエルゴカルシフェロールもまた、25-ヒドロキシル化されて25-ヒドロキシエルゴカルシフェロール(エルカルシジオール、25(OH)D2)を形成することができる;両方の形態は、血中では25(OH)Dとして一緒に測定される。
At a typical intake of cholecalciferol (up to 2000 IU/day), conversion to calcifediol is rapid. When large doses are given (100,000 IU), it takes 7 days to reach peak calcifediol concentrations. Calcifediol binds in the blood to vitamin D-binding protein (also known as gc-globulin) and is the main circulating vitamin D metabolite. Calcifediol has an elimination half-life of around 15 to 30 days.
Calcifediol is further hydroxylated at the 1-alpha-position in the kidneys to form 1,25-(OH)2D3, calcitriol. This enzymatic 25(OH)D-1α-hydroxylase reaction is performed exclusively by CYP27B1, which is highly expressed in the kidneys where it is principally regulated by parathyroid hormone, but also by FGF23 and calcitriol itself. CYP27B1 is also expressed in a number of other tissues, including macrophages, monocytes, keratinocytes, placenta and parathyroid gland and extra-renal synthesis of calcitriol from calcifediol has been shown to have biological effects in these tissues.
Calcifediol is also converted into 24,25-dihydroxycholecalciferol by 24-hydroxylation. This enzymatic reaction is performed by CYP24A1 which is expressed in many vitamin D target tissues including kidney, and is induced by calcitriol. This will inactivate calcitriol to calcitroic acid, but 24,25-(OH)2D3 may have some biological actions itself.
Blood test for vitamin D deficiency
In medical practice, a blood test for 25-hydroxy-vitamin D, 25(OH)D, is used to determine an individual's vitamin D status. The name 25(OH)D refers to any combination of calcifediol (25-hydroxy-cholecalciferol), derived from vitamin D3, and ercalcidiol (25-hydroxy-ergocalciferol), derived from vitamin D2. The first of these (also known as 25-hydroxy vitamin D3) is made by the body, or is sourced from certain animal foods or cholecalciferol supplements. The second (25-hydroxy vitamin D2) is from certain vegetable foods or ergocalciferol supplements.
This measurement is considered the best indicator of overall vitamin D status. US labs generally report 25(OH)D levels as ng/mL. Other countries use nmol/L. Multiply ng/mL by 2.5 to convert to nmol/L.
This test can be used to diagnose vitamin D deficiency, and is performed in people with high risk for vitamin D deficiency, when the results of the test can be used to support beginning replacement therapy with vitamin D supplements. Patients with osteoporosis, chronic kidney disease, malabsorption, obesity, and some other infections may be at greater risk for being vitamin D-deficient and so are more likely to have this test. Although vitamin D deficiency is common in some populations including those living at higher latitudes or with limited sun exposure, the 25(OH)D test is not usually requested for the entire population. Physicians may advise low risk patients to take over-the-counter vitamin D supplements in place of having screening.
It is the most sensitive measure, though experts have called for improved standardization and reproducibility across different laboratories. According to MedlinePlus, the recommended range of 25(OH)D is 20 to 40 ng/mL (50 to 100 nmol/L) though they recognize many experts recommend 30 to 50 ng/mL (75 to 125 nmol/L). The normal range varies widely depending on several factors, including age and geographic location. A broad reference range of 20 to 150 nmol/L (8-60 ng/mL) has also been suggested, while other studies have defined levels below 80 nmol/L (32 ng/mL) as indicative of vitamin D deficiency.
Increasing calcifediol levels up to levels of 80 nmol/L (32 ng/mL) are associated with increasing the fraction of calcium that is absorbed from the gut. Urinary calcium excretion balances intestinal calcium absorption and does not increase with calcifediol levels up to ~400 nmol/L (160 ng/mL).
Supplementation
Calcifediol supplements have been used in some studies to improve vitamin D status. Indications for their use include vitamin D deficiency or insufficiency, refractory rickets (vitamin D resistant rickets), familial hypophosphatemia, hypoparathyroidism, hypocalcemia and renal osteodystrophy and, with calcium, in primary or corticosteroid-induced osteoporosis.
Calcifediol may have advantages over cholecalciferol for the correction of vitamin D deficiency states. A review of the results of nine randomized control trials which compared oral doses of both, found that calcifediol was 3.2-fold more potent than cholecalciferol. Calcifediol is better absorbed from the intestine and has greater affinity for the vitamin-D-binding protein, both of which increase its bioavailability. Orally administered calcifediol has a much shorter half-life with faster elimination. These properties may be beneficial in people with intestinal malabsorption, obesity, or treated with certain other medications.
In 2016, the FDA approved a formulation of calcifediol (Rayaldee) 60 microgram daily as a prescription medication to treat secondary hyperparathyroidism in patients with chronic kidney disease.
Interactive pathway map
Click on genes, proteins and metabolites below to link to respective articles. [§ 1]
- ↑ The interactive pathway map can be edited at WikiPathways: "VitaminDSynthesis_WP1531".
History
Research in the laboratory of Hector DeLuca identified 25(OH)D in 1968 and showed that the liver was necessary for its formation. The enzyme responsible for this synthesis, cholecalciferol 25-hydroxylase, was isolated in the same laboratory by Michael F. Holick in 1972.
研究
骨粗鬆症の予防と治療において、カルシフェジオールとコレカルシフェロールを含む他のビタミンDの効果を比較する研究が進行中である。