ナイアシン
Niacin/ja
ナイアシン(niacin)は、有機化合物の一種で、ビタミン B3のビタマーであり、必須人体栄養素である。動植物がアミノ酸トリプトファンから生成する。ナイアシンは様々なホールフードや加工食品から食事中に摂取されるが、強化食品の含有量が最も高い。包装食品、肉類、鶏肉、マグロやサケなどの赤身魚に最も多く含まれ、ナッツ類、豆類、種子類に含まれる量は少ない。栄養補助食品としてのナイアシンは、ナイアシン欠乏によって引き起こされる疾患であるペラグラの治療に用いられる。ペラグラの徴候や症状には、皮膚や口の病変、貧血、頭痛、疲労感などがある。多くの国では、小麦粉や他の食用穀物への添加を義務付けており、それによってペラグラのリスクを減らしている。
| |||
| Names | |||
|---|---|---|---|
| Pronunciation | /ˈnaɪəsɪn/ | ||
| Preferred IUPAC name
Pyridine-3-carboxylic acid | |||
Other names
| |||
| Identifiers | |||
3D model (JSmol)
|
|||
| 3DMet | |||
| 109591 | |||
| ChEBI | |||
| ChEMBL | |||
| ChemSpider | |||
| DrugBank | |||
| EC Number |
| ||
| 3340 | |||
| KEGG | |||
| MeSH | Niacin | ||
PubChem CID
|
|||
| RTECS number |
| ||
| UNII | |||
| |||
| |||
| Properties | |||
| C6H5NO2 | |||
| Molar mass | 123.111 g·mol−1 | ||
| Appearance | White, translucent crystals | ||
| Density | 1.473 g cm−3 | ||
| Melting point | 237 °C; 458 °F; 510 K | ||
| 18 g L−1 | |||
| log P | 0.219 | ||
| Acidity (pKa) | 2.0, 4.85 | ||
| Isoelectric point | 4.75 | ||
Refractive index (nD)
|
1.4936 | ||
| 0.1271305813 D | |||
| Thermochemistry | |||
Std enthalpy of
formation (ΔfH⦵298) |
−344.9 kJ mol−1 | ||
Std enthalpy of
combustion (ΔcH⦵298) |
−2.73083 MJ mol−1 | ||
| Pharmacology | |||
| C04AC01 (WHO) C10BA01 (WHO) C10AD02 (WHO) C10AD52 (WHO) | |||
| License data |
| ||
| 筋肉内、経口 | |||
| Pharmacokinetics: | |||
| 20–45 min | |||
| Hazards | |||
| GHS labelling: | |||

| |||
| Warning | |||
| H319 | |||
| P264, P280, P305+P351+P338, P337+P313, P501 | |||
| NFPA 704 (fire diamond) | |||
| Flash point | 193 °C (379 °F; 466 K) | ||
| 365 °C (689 °F; 638 K) | |||
| Clinical data | |
|---|---|
| Trade names | Niacor, Niaspan, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682518 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | 筋肉内、経口 |
| Legal status | |
| Legal status |
|
| Identifiers | |
| PDB ligand | |
アミド誘導体ニコチンアミド(ナイアシンアミド)は、補酵素ニコチンアミドアデニンジヌクレオチド(NAD)とニコチンアミドアデニンジヌクレオチドリン酸(NADP+)の構成成分である。ナイアシンとニコチンアミドはビタミン活性において同一であるが、ニコチンアミドはナイアシンのような薬理学的、脂質修飾作用や副作用を持たない、すなわち、ナイアシンが-アミド基を取る場合、コレステロールを減少させることも潮紅を引き起こすこともない。ニコチンアミドはナイアシン欠乏症の治療薬として推奨されるが、その理由は、副作用とされる潮紅を起こすことなく、治療量を投与することができるからである。
ナイアシンも処方医薬品である。ビタミン機能の食事摂取推奨量をはるかに超える量は、血中トリグリセリドと低密度リポ蛋白コレステロール(LDL-C)を低下させ、血中高密度リポ蛋白コレステロール(HDL-C、しばしば「善玉」コレステロールと呼ばれる)を上昇させる。即放性ナイアシンと徐放性ナイアシンの2種類がある。最初の処方量は500 mg/日で、治療効果が得られるまで時間をかけて増量する。即時放出型は3,000 mg/日、徐放型は2,000 mg/日という高用量が可能である。脂質の変化が証明されているにもかかわらず、ナイアシンはすでにスタチンを服用している人の心血管系疾患のリスクを減少させるのに有用であるとは認められていない。2010年のレビューでは、ナイアシンは単剤療法として有効であると結論付けられていたが、2倍の臨床試験を組み込んだ2017年のレビューでは、処方ナイアシンは脂質値に影響を及ぼすものの、全死亡、心血管死亡、心筋梗塞、致死的または非致死的脳卒中を減少させなかったと結論付けられた。処方ナイアシンは肝毒性を引き起こし、2型糖尿病のリスクを増加させることが示された。米国におけるナイアシンの処方は、2009年の9.4 万人をピークに、2020年までに800 万人まで減少した。
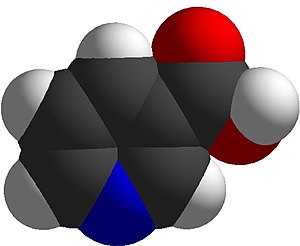
ナイアシンは式を持つ。C
6H
5NO
2で、ピリジンカルボン酸のグループに属する。ニコチンアミドアデニンジヌクレオチドとニコチンアミドアデニンジヌクレオチドリン酸の前駆体として、ナイアシンはDNA修復に関与する。
定義
ナイアシンはビタミン、すなわち必須栄養素であり、栄養補助食品として、また米国では処方薬として販売されている。ビタミンとしては、補酵素ニコチンアミドアデニンジヌクレオチド(NAD)とニコチンアミドアデニンジヌクレオチドリン酸(NADP)の前駆体である。これらの化合物は多くの脱水素酵素の補酵素であり、多くの水素移動過程に関与している。NADは脂肪、炭水化物、タンパク質、アルコールの異化、細胞シグナル伝達、DNA修復において重要であり、NADPは主に脂肪酸やコレステロール合成などの同化反応において重要である。いくつかの国が推奨するビタミン摂取量は、健康な成人の必要量を満たすには14~18 mg/日で十分であるとしている。ナイアシンだけでなく、ニコチンアミド(ナイアシンアミド)も、ビタミンの欠乏によって引き起こされる病気であるペラグラの予防と治療に用いられる。ナイアシンをコレステロールとトリグリセリドの上昇の治療薬として用いる場合、1日の投与量は500~3,000 mg/日である。高用量のニコチンアミドはこの薬効はない。
ビタミン欠乏症
食事中のナイアシンの深刻な欠乏はペラグラという病気を引き起こし、下痢、皮膚の色素沈着と肥厚を伴う日光過敏性皮膚炎(画像参照)、口と舌の炎症、せん妄、痴呆を特徴とし、放置すると死に至る。一般的な精神症状には、いらいら、集中力の低下、不安、疲労、記憶力の低下、落ち着きのなさ、無気力、抑うつなどがある。欠乏によって神経変性が起こる生化学的メカニズムはよくわかっていないが、次のようなことが考えられる: A) ニコチンアミドアデニンジヌクレオチド(NAD+)が神経毒性のトリプトファン代謝物の生成を抑制するために必要である; C)、ポリ(ADP-リボース)ポリメラーゼ(PARP)経路の活性化。PARPはDNA修復に関与する核内酵素であるが、NAD+がない場合は細胞死につながる。D)神経保護作用のある脳由来神経栄養因子またはその受容体トロポミオシン受容体キナーゼBの合成の減少、あるいはE)ナイアシン欠乏に直接起因するゲノム発現の変化。
ナイアシン欠乏症は先進国ではほとんど見られず、貧困や栄養失調、慢性的なアルコール中毒による二次的な栄養失調と関連するのが一般的である。また、トウモロコシは消化可能なナイアシンが少ない唯一の穀物であるため、トウモロコシ(とうもろこし)を主食としている低開発地域で起こる傾向がある。ニクスタマリゼーションと呼ばれる調理技術、すなわちアルカリ成分による前処理は、トウモロコシミール/小麦粉製造時にナイアシンの生物学的利用能を高める。このため、トウモロコシをトルティーヤやホミニーとして食べる人は、ナイアシン欠乏症のリスクが少ない。
世界保健機関(WHO)は、欠乏症の治療には、ナイアシンの代わりにナイアシンアミド、すなわちニコチンアミドを投与することを推奨している。ガイドラインでは、300 mg/日を3〜4週間使用することを推奨している。認知症と皮膚炎は1週間以内に改善がみられる。他のビタミンB群の欠乏も考えられるため、WHOはナイアシンアミドに加えてマルチビタミンの摂取を推奨している。
ハートナップ病は、ナイアシン欠乏をもたらす遺伝性栄養障害である。ナイアシン合成の前駆体である必須アミノ酸トリプトファンの吸収不全をもたらす遺伝的障害を持つイギリスの家族にちなんで名付けられた。症状はペラグラに似ており、赤い鱗状の発疹や日光に過敏になる。この疾患の治療法として、ナイアシンまたはナイアシンアミドを1回50~100mg、1日2回経口投与するが、早期に発見し治療すれば予後は良好である。ナイアシン合成はカルチノイド症候群でも欠損しているが、これはその前駆体の代謝的転用のためである。セロトニンを形成するためにトリプトファンが代謝転換されるためである。
ビタミンの状態を測定する
ナイアシンおよびナイアシン代謝物の血漿中濃度は、ナイアシンの状態を示す有用なマーカーではない。メチル化代謝物N1-メチルニコチンアミドの尿中排泄は、信頼性が高く、感度が高いと考えられている。測定には24時間採尿が必要である。成人の場合、5.8μmol/日未満はナイアシンの欠乏状態、5.8~17.5μmol/日は低値を示す。世界保健機関(WHO)によると、尿中N1-メチルニコチンアミドを表す代替手段は、24時間採尿におけるmg/gクレアチニンであり、欠乏は0.5未満、低は0.5~1.59、許容は1.6~4.29、高は4.3以上と定義されている。 ナイアシンの欠乏は、ペラグラの徴候や症状が現れる前に起こる。赤血球のニコチンアミドアデニンジヌクレオチド(NAD)濃度は、ナイアシン欠乏のもうひとつの鋭敏な指標となる可能性があるが、欠乏、低値、適正の定義は確立されていない。最後に、低ナイアシン食では血漿トリプトファンが減少するが、これはトリプトファンがナイアシンに変換されるためである。しかし、トリプトファンの低下は、この必須アミノ酸の少ない食事によっても起こりうるので、ビタミンの状態の確認に特異的なものではない。
食事に関する推奨事項
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
米国医学研究所(2015年に米国医学アカデミーに改称)は、1998年にナイアシンの推定平均必要量(EAR)と推奨食事許容量(RDA)を更新し、耐容上限摂取量レベル(UL)も更新した。RDAの代わりに、ほとんどの人の栄養所要量を満たすのに十分な食事摂取レベルを特定する十分な証拠がない集団について、十分摂取量(AAI)が特定される。(表参照)。
欧州食品安全機関(EFSA)は、RDAの代わりに母集団基準摂取量(PRI)、EARの代わりに平均必要量を用い、これらの情報をまとめて食事摂取基準値(DRV)と呼んでいる。EUでは、単位がmg/日ではなく、消費エネルギー1メガジュール(MJ)あたりのミリグラムであることを除き、AIとULは米国と同じ定義である。女性(妊娠中または授乳中を含む)、男性、小児の場合、PRIは1メガジュールあたり1.6 mgである。1MJ=239kcalに換算すると、2390キロカロリーを消費する成人は、16 mgのナイアシンを摂取することになる。これは米国のRDA(成人女性14 mg/日、成人男性16 mg/日)に匹敵する。
ULは、有害な影響を引き起こすビタミンやミネラルの量を特定し、"健康への有害な影響を引き起こしそうにない1日の最大摂取量 "を上限値として選択することで設定される。各国の規制機関は必ずしも一致していない。米国では、ティーンエイジャーと成人は30または35mg、子供はそれ以下である。EFSAの成人のULは10 mg/日とされており、これは米国の値の約3分の1である。政府のULはすべて、ナイアシンをサプリメントとして一度に摂取する場合に適用されるもので、皮膚紅潮反応を避けるための制限値として意図されている。このため、EFSAでは、1日の推奨摂取量がULよりも高くなることがある。
DRIもDRVも、必要量をナイアシン当量(NE)として表記しており、1 mg NE = 1 mgのナイアシンまたは60 mgの必須アミノ酸トリプトファンとして計算される。これは、アミノ酸がビタミンの合成に利用されるためである。
米国の食品および栄養補助食品の表示目的では、1食分の量はデイリーバリュー(%DV)のパーセントで表される。ナイアシンの表示目的では、1日当たりの価値の100%は16 mgである。2016年5月27日以前は20 mgであったが、RDAと一致させるために改訂された。 更新された表示規制への準拠は、年間食品売上高がUS$10 百万以上の製造業者には2020年1月1日までに、それ以下の製造業者には2021年1月1日までに義務付けられた。新旧の成人一日摂取量の表は基準一日摂取量に掲載されている。
摂取源
ナイアシンは、強化パッケージ食品を含む様々なホールフードや加工食品、様々な動物由来の肉、魚介類、香辛料などに含まれている。一般に、動物性食品は1食あたり約5~10 mgのナイアシンを供給するが、乳製品や卵にはほとんど含まれない。ナッツ類、豆類、穀類などの植物性食品では、1食あたり約2~5 mgのナイアシンが摂取できるが、穀類製品の中には、天然に存在するナイアシンの大部分が多糖類や糖ペプチドと結合しており、生物学的利用率が約30%しかないものもある。小麦粉などの強化食品にはナイアシンが添加されており、これは生物学的に利用可能である。100グラムあたりのナイアシン含有量が最も高い全食品源は以下の通りである:
| 摂取源 | 量 (mg / 100g) |
|---|---|
| Nutritional yeast/ja 1人分 = 大さじ2杯 (16 g)に56 mgが含まれる |
350 |
| Tuna/ja, キハダ | 22.1 |
| Peanut/ja | 14.3 |
| Peanut butter/ja | 13.1 |
| Bacon/ja | 10.4 |
| Tuna/ja, ライト, 缶詰 | 10.1 |
| Salmon/ja | 10.0 |
| ターキー どの部分をどのように調理するかによる | 7-12 |
| 鶏 どの部分をどのように調理するかによる | 7-12 |
| 摂取源 | 量 (mg / 100g) |
|---|---|
| 牛肉 どの部分をどのように調理するかによる | 4-8 |
| 豚肉 どの部分をどのように調理するかによる | 4-8 |
| Sunflower seeds/ja | 7.0 |
| Tuna/ja, ホワイト, 缶詰 | 5.8 |
| Almond/ja | 3.6 |
| Mushroom/ja, ホワイト | 3.6 |
| タラ | 2.5 |
| 玄米 | 2.5 |
| Hot dog/ja | 2.0 |
| 摂取源 | 量 (mg / 100g) |
|---|---|
| Avocado/ja | 1.7 |
| Potato/ja, 焼き、皮付き | 1.4 |
| コーン (とうもろこし) | 1.0 |
| 白米 | 0.5 |
| Kale/ja | 0.4 |
| 卵 | 0.1 |
| Milk/ja | 0.1 |
| チーズ | 0.1 |
| 豆腐 | 0.1 |
栄養酵母、ピーナッツ、ピーナッツバター、タヒニ、玄米、マッシュルーム、アボカド、ヒマワリの種などの製品が含まれていれば、ベジタリアンやビーガンの食事で十分な量を摂取することができる。十分な摂取量を確保するために、強化食品や栄養補助食品を摂取することもできる。
食品の調理法
食品に自然に含まれるナイアシンは、高熱調理、特に酸性の食品やソースの存在下で破壊されやすい。ナイアシンは水に溶けるので、水で煮た食品からも失われる可能性がある。
食品強化
各国は、既知の欠乏症に対処するため、食品に栄養素を強化している。2020年現在、54カ国が小麦粉にナイアシンまたはナイアシンアミドの食品強化を義務付けており、14カ国がトウモロコシ粉、6カ国が米の食品強化を義務付けている。国によって、ナイアシンの強化量は1.3~6.0mg/100gの幅がある。
As a dietary supplement
In the United States, niacin is sold as a non-prescription dietary supplement with a range of 100 to 1000 mg per serving. These products often have a Structure/Function health claim allowed by the US Food & Drug Administration (FDA). An example would be "Supports a healthy blood lipid profile." The American Heart Association strongly advises against the substitution of dietary supplement niacin for prescription niacin because of potentially serious side effects, which means that niacin should only be used under the supervision of a health care professional, and because manufacture of dietary supplement niacin is not as well-regulated by the FDA as prescription niacin. More than 30 mg niacin consumed as a dietary supplement can cause skin flushing. Face, arms and chest skin turns a reddish color because of vasodilation of small subcutaneous blood vessels, accompanied by sensations of heat, tingling and itching. These signs and symptoms are typically transient, lasting minutes to hours; they are considered unpleasant rather than toxic.
As lipid-modifying medication
In the United States, prescription niacin, in immediate-release and slow-release forms, is used to treat primary hyperlipidemia and hypertriglyceridemia. It is used either as a monotherapy or in combination with other lipid-modifying drugs. Dosages start at 500 mg/day and are often gradually increased to as high as 3000 mg/day for immediate release or 2000 mg/day for slow release (also referred to as sustained release) to achieve the targeted lipid changes (lower LDL-C and triglycerides, and higher HDL-C). Prescriptions in the US peaked in 2009, at 9.4 million and had declined to 800 thousand by 2020.
Systematic reviews found no effect of prescription niacin on all-cause mortality, cardiovascular mortality, myocardial infarctions, nor fatal or non-fatal strokes despite raising HDL cholesterol. Reported side effects include an increased risk of new-onset type 2 diabetes.
Mechanisms
Niacin reduces synthesis of low-density lipoprotein cholesterol (LDL-C), very low-density lipoprotein cholesterol (VLDL-C), lipoprotein(a) and triglycerides, and increases high-density lipoprotein cholesterol (HDL-C). The lipid-therapeutic effects of niacin are partly mediated through the activation of G protein-coupled receptors, including hydroxycarboxylic acid receptor 2 (HCA2)and hydroxycarboxylic acid receptor 3 (HCA3), which are highly expressed in body fat. HCA2 and HCA3 inhibit cyclic adenosine monophosphate (cAMP) production and thus suppress the release of free fatty acids (FFAs) from body fat, reducing their availability to the liver to synthesize the blood-circulating lipids in question. A decrease in free fatty acids also suppresses liver expression of apolipoprotein C3 and PPARg coactivator-1b, thus increasing VLDL-C turnover and reducing its production. Niacin also directly inhibits the action of diacylglycerol O-acyltransferase 2 (DGAT2) a key enzyme for triglyceride synthesis.
The mechanism behind niacin increasing HDL-C is not totally understood, but seems to occur in various ways. Niacin increases apolipoprotein A1 levels by inhibiting the breakdown of this protein, which is a component of HDL-C. It also inhibits HDL-C hepatic uptake by suppressing production of the cholesterol ester transfer protein (CETP) gene. It stimulates the ABCA1 transporter in monocytes and macrophages and upregulates peroxisome proliferator-activated receptor gamma, resulting in reverse cholesterol transport.
Combined with statins
Extended release niacin was combined with lovastatin (Advicor), and with simvastatin (Simcor), as prescription drug combinations. The combination niacin/lovastatin was approved by the U.S. Food and Drug Administration (FDA) in 2001. The combination niacin/simvastatin was approved by the FDA in 2008. Subsequently, large outcome trials using these niacin and statin therapies were unable to demonstrate incremental benefit of niacin beyond statin therapy alone. The FDA withdrew approval of both drugs in 2016. The reason given: "Based on the collective evidence from several large cardiovascular outcome trials, the Agency has concluded that the totality of the scientific evidence no longer supports the conclusion that a drug-induced reduction in triglyceride levels and/or increase in HDL-cholesterol levels in statin-treated patients results in a reduction in the risk of cardiovascular events." The drug company discontinued the drugs.
Contraindications
Prescription immediate release (Niacor) and extended release (Niaspan) niacin are contraindicated for people with either active or a history of liver disease because both, but especially Niaspan, have been associated with instances of serious, on occasion fatal, liver failure. Both products are contraindicated for people with existing peptic ulcer disease, or other bleeding problems because niacin lowers platelet count and interferes with blood clotting. Both products are also contraindicated for women who are pregnant or expecting to become pregnant because safety during pregnancy has not been evaluated in human trials. These products are contraindicated for women who are lactating because it is known that niacin is excreted into human milk, but the amount and potential for adverse effects in the nursing infant are not known. Women are advised to either not nurse their child or discontinue the drug. High-dose niacin has not been tested or approved for use in children under 16 years.
Adverse effects
The most common adverse effects of medicinal niacin (500–3000 mg) are flushing (e.g., warmth, redness, itching or tingling) of the face, neck and chest, headache, abdominal pain, diarrhea, dyspepsia, nausea, vomiting, rhinitis, pruritus and rash. These can be minimized by initiating therapy at low dosages, increasing dosage gradually, and avoiding administration on an empty stomach.
The acute adverse effects of high-dose niacin therapy (1–3 grams per day) – which is commonly used in the treatment of hyperlipidemias – can further include hypotension, fatigue, glucose intolerance and insulin resistance, heartburn, blurred or impaired vision, and macular edema. With long-term use, the adverse effects of high-dose niacin therapy (750 mg per day) also include liver failure (associated with fatigue, nausea, and loss of appetite), hepatitis, and acute liver failure; these hepatotoxic effects of niacin occur more often when extended-release dosage forms are used. The long-term use of niacin at greater than or equal to 2 grams per day also significantly increases the risk of cerebral hemorrhage, ischemic stroke, gastrointestinal ulceration and bleeding, diabetes, dyspepsia, and diarrhea.
Flushing
Flushing – a short-term dilatation of skin arterioles, causing reddish skin color – usually lasts for about 15 to 30 minutes, although sometimes can persist for weeks. Typically, the face is affected, but the reaction can extend to neck and upper chest. The cause is blood vessel dilation due to elevation in prostaglandin GD2 (PGD2) and serotonin. Flushing was often thought to involve histamine, but histamine has been shown not to be involved in the reaction. Flushing is sometimes accompanied by a prickly or itching sensation, in particular, in areas covered by clothing.
Prevention of flushing requires altering or blocking the prostaglandin-mediated pathway. Aspirin taken half an hour before the niacin prevents flushing, as does ibuprofen. Taking niacin with meals also helps reduce this side effect. Acquired tolerance will also help reduce flushing; after several weeks of a consistent dose, most people no longer experience flushing. Slow- or "sustained"-release forms of niacin have been developed to lessen these side effects.
Liver damage
Niacin in medicinal doses can cause modest elevations in serum transaminase and unconjugated bilirubin, both biomarkers of liver injury. The increases usually resolve even when drug intake is continued. However, less commonly, the sustained release form of the drug can lead to serious hepatotoxicity, with onset in days to weeks. Early symptoms of serious liver damage include nausea, vomiting and abdominal pain, followed by jaundice and pruritus. The mechanism is thought to be a direct toxicity of elevated serum niacin. Lowering dose or switching to the immediate release form can resolve symptoms. In rare instances the injury is severe, and progresses to liver failure.
Diabetes
The high doses of niacin used to treat hyperlipidemia have been shown to elevate fasting blood glucose in people with type 2 diabetes. Long-term niacin therapy was also associated with an increase in the risk of new-onset type 2 diabetes.
Other adverse effects
High doses of niacin can also cause niacin maculopathy, a thickening of the macula and retina, which leads to blurred vision and blindness. This maculopathy is reversible after niacin intake ceases. Niaspan, the slow-release product, has been associated with a reduction in platelet content and a modest increase in prothrombin time.
Pharmacology
Pharmacodynamics
Activating HCA2 has effects other than lowering serum cholesterol and triglyceride concentrations: antioxidative, anti-inflammatory, antithrombotic, improved endothelial function and plaque stability, all of which counter development and progression of atherosclerosis.
Niacin inhibits cytochrome P450 enzymes CYP2E1, CYP2D6 and CYP3A4. Niacin produces a rise in serum unconjugated bilirubin in normal individuals and in those with Gilbert's Syndrome. However, in the Gilbert's Syndrome, the rise in bilirubin is higher and clearance is delayed longer than in normal people. One test used to aid in diagnosing Gilbert's Syndrome involves intravenous administration of nicotinic acid (niacin) in a dose of 50 mg over a period of 30 seconds.
Pharmacokinetics
Both niacin and niacinamide are rapidly absorbed from the stomach and small intestine. Absorption is facilitated by sodium-dependent diffusion, and at higher intakes, via passive diffusion. Unlike some other vitamins, the percent absorbed does not decrease with increasing dose, so that even at amounts of 3-4 grams, absorption is nearly complete. With a one gram dose, peak plasma concentrations of 15 to 30 μg/mL are reached within 30 to 60 minutes. Approximately 88% of an oral pharmacologic dose is eliminated by the kidneys as unchanged niacin or nicotinuric acid, its primary metabolite. The plasma elimination half-life of niacin ranges from 20 to 45 minutes.
Niacin and nicotinamide are both converted into the coenzyme NAD. NAD converts to NADP by phosphorylation in the presence of the enzyme NAD+ kinase. High energy requirements (brain) or high turnover rate (gut, skin) organs are usually the most susceptible to their deficiency. In the liver, niacinamide is converted to storage nicotinamide adenine dinucleotide (NAD). As needed, liver NAD is hydrolyzed to niacinamide and niacin for transport to tissues, there reconverted to NAD to serve as an enzyme cofactor. Excess niacin is methylated in the liver to N1-methylnicotinamide (NMN) and excreted in urine as such or as the oxidized metabolite N1-methyl-2-pyridone-5-carboxamide (2-pyridone). Decreased urinary content of these metabolites is a measure of niacin deficiency.
Production
Biosynthesis
In addition to absorbing niacin from diet, niacin can be synthesized from the essential amino acid tryptophan, a five-step process with the penultimate compound being quinolinic acid (see figure). Some bacteria and plants utilize aspartic acid in a pathway that also goes to quinolinic acid. For humans, the efficiency of conversion is estimated as requiring 60 mg of tryptophan to make 1 mg of niacin. Riboflavin, vitamin B6 and iron are required for the process. Pellagra is a consequence of a corn-dominant diet because the niacin in corn is poorly bioavailable and corn proteins are low in tryptophan compared to wheat and rice proteins.
Industrial synthesis
Nicotinic acid was first synthesized in 1867 by oxidative degradation of nicotine with potassium chromate and sulfuric acid — this is the origin of the name. Niacin is prepared by hydrolysis of nicotinonitrile, which, as described above, is generated by oxidation of 3-picoline. Oxidation can be effected by air, but ammoxidation is more efficient. In the latter process, nicotinonitrile is produced by ammoxidation of 3-methylpyridine. Nitrile hydratase is then used to catalyze nicotinonitrile to nicotinamide, which can be converted to niacin. Alternatively, ammonia, acetic acid and paraldehyde are used to make 5-ethyl-2-methyl-pyridine, which is then oxidized to niacin. New "greener" catalysts are being tested using manganese-substituted aluminophosphates that use acetyl peroxyborate as non-corrosive oxidant, avoiding producing nitrogen oxides as do traditional ammoxidations.
The demand for commercial production includes for animal feed and for food fortification meant for human consumption. According to Ullmann's Encyclopedia of Industrial Chemistry, worldwide 31,000 tons of nicotinamide were sold in 2014.
Climate Impact
The production of niacin creates nitrous oxide as a by-product, which is a potent greenhouse gas. In 2018, it was discovered that a niacin factory in Visp, Switzerland, was responsible for around one percent of the country's greenhouse gas emissions. Eventually, catalytic scrubbing technology that avoids most of the emissions was installed in 2021.
Chemistry
This colorless, water-soluble solid is a derivative of pyridine, with a carboxyl group (COOH) at the 3-position. Other forms of vitamin B3 include the corresponding amide nicotinamide (niacinamide), where the carboxyl group has been replaced by a carboxamide group (CONH
2).
Preparations
Niacin is incorporated into multi-vitamin and sold as a single-ingredient dietary supplement. The latter can be immediate or slow release.
Nicotinamide (niacinamide) is used to treat niacin deficiency because it does not cause the flushing adverse reaction seen with niacin. Nicotinamide may be toxic to the liver at doses exceeding 3 g/day for adults.
Prescription products can be immediate release (Niacor, 500 mg tablets) or extended release (Niaspan, 500 and 1000 mg tablets). Niaspan has a film coating that delays release of the niacin, resulting in an absorption over a period of 8–12 hours. This reduces vasodilation and flushing side effects, but increases the risk of hepatotoxicity compared to the immediate release drug.
Prescription niacin preparations in combination with statin drugs (discontinued) are described above. A combination of niacin and laropiprant had been approved for use in Europe and marketed as Tredaptive. Laropiprant is a prostaglandin D2 binding drug shown to reduce niacin-induced vasodilation and flushing side effects. A clinical trial showed no additional efficacy of Tredaptive in lowering cholesterol when used together with other statin drugs, but did show an increase in other side effects. The study resulted in the withdrawal of Tredaptive from the international market.
One form of dietary supplement sold in the US is inositol hexanicotinate (IHN), also called inositol nicotinate. This is inositol that has been esterified with niacin on all six of inositol's alcohol groups. IHN is usually sold as "flush-free" or "no-flush" niacin in units of 250, 500, or 1000 mg/tablets or capsules. In the US, it is sold as an over-the-counter formulation, and often is marketed and labeled as niacin, thus misleading consumers into thinking they are getting an active form of the medication. While this form of niacin does not cause the flushing associated with the immediate-release products, there is not enough evidence to recommend IHN to treat hyperlipidemia.
History
Niacin as a chemical compound was first described by chemist Hugo Weidel in 1873 in his studies of nicotine, but that predated by many years the concept of food components other than protein, fat and carbohydrates that were essential for life. Vitamin nomenclature was initially alphabetical, with Elmer McCollum calling these fat-soluble A and water-soluble B. Over time, eight chemically distinct, water-soluble B vitamins were isolated and numbered, with niacin as vitamin B3.
Corn (maize) became a staple food in the southeast United States and in parts of Europe. A disease that was characterized by dermatitis of sunlight-exposed skin was described in Spain in 1735 by Gaspar Casal. He attributed the cause to poor diet. In northern Italy it was named "pellagra" from the Lombard language (agra = holly-like or serum-like; pell = skin). In time, the disease was more closely linked specifically to corn. In the US, Joseph Goldberger was assigned to study pellagra by the Surgeon General of the United States. His studies confirmed a corn-based diet as the culprit, but he did not identify the root cause.
Nicotinic acid was extracted from liver by biochemist Conrad Elvehjem in 1937. He later identified the active ingredient, referring to it as "pellagra-preventing factor" and the "anti-blacktongue factor." It was also referred to as "vitamin PP", "vitamin P-P" and "PP-factor", all derived from the term "pellagra-preventive factor". In the late 1930s, studies by Tom Douglas Spies, Marion Blankenhorn, and Clark Cooper confirmed that niacin cured pellagra in humans. The prevalence of the disease was greatly reduced as a result. Nicotinic acid was initially synthesized by oxidizing nicotine with potassium chromate and sulfuric acid. Hence, in 1942, when flour enrichment with nicotinic acid began, a headline in the popular press said "Tobacco in Your Bread." In response, the Council on Foods and Nutrition of the American Medical Association approved of the Food and Nutrition Board's new names niacin and niacin amide for use primarily by non-scientists. It was thought appropriate to choose a name to dissociate nicotinic acid from nicotine, to avoid the perception that vitamins or niacin-rich food contains nicotine, or that cigarettes contain vitamins. The resulting name niacin was derived from nicotinic acid + vitamin.
Carpenter found in 1951, that niacin in corn is biologically unavailable, and can be released only in very alkaline lime water of pH 11. This explains why a Latin-American culture that used alkali-treated cornmeal to make tortilla was not at risk for niacin deficiency.
In 1955, Altschul and colleagues described large amounts of niacin as having a lipid-lowering property. As such, niacin is the oldest known lipid-lowering drug. Lovastatin, the first 'statin' drug, was first marketed in 1987.
Research
In animal models and in vitro, niacin produces marked anti-inflammatory effects in a variety of tissues – including the brain, gastrointestinal tract, skin, and vascular tissue – through the activation of hydroxycarboxylic acid receptor 2 (HCA2), also known as niacin receptor 1 (NIACR1). Unlike niacin, nicotinamide does not activate NIACR1; however, both niacin and nicotinamide activate the G protein-coupled estrogen receptor (GPER) in vitro.
External links
- "Niacin". Drug Information Portal. U.S. National Library of Medicine.
| この記事は、クリエイティブ・コモンズ・表示・継承ライセンス3.0のもとで公表されたウィキペディアの項目Niacin/ja(7 January 2024編集記事参照)を素材として二次利用しています。 Lua error in Module:Itemnumber at line 91: attempt to concatenate local 'qid' (a nil value). |


