Dipeptidyl peptidase-4 inhibitor: Difference between revisions
Marked this version for translation |
|||
| (One intermediate revision by the same user not shown) | |||
| Line 1: | Line 1: | ||
<languages /> | |||
<translate> | |||
<!--T:1--> | |||
{{Short description|Enzyme blocker and diabetes treatment drug}} | {{Short description|Enzyme blocker and diabetes treatment drug}} | ||
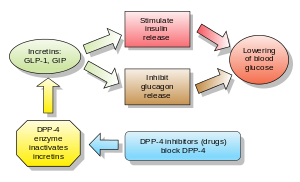
[[Image:Incretins and DPP 4 inhibitors.svg|thumb|300px|right|DPP-4 inhibitors and GLP-1]] | [[Image:Incretins and DPP 4 inhibitors.svg|thumb|300px|right|DPP-4 inhibitors and GLP-1]] | ||
<!--T:2--> | |||
'''Inhibitors of dipeptidyl peptidase 4''' ('''DPP-4 inhibitors''' or '''gliptins''') are a class of [[oral hypoglycemic]]s that [[Enzyme inhibitors|block]] the [[enzyme]] [[dipeptidyl peptidase-4]] (DPP-4). They can be used to treat [[diabetes mellitus type 2]]. | '''Inhibitors of dipeptidyl peptidase 4''' ('''DPP-4 inhibitors''' or '''gliptins''') are a class of [[oral hypoglycemic]]s that [[Enzyme inhibitors|block]] the [[enzyme]] [[dipeptidyl peptidase-4]] (DPP-4). They can be used to treat [[diabetes mellitus type 2]]. | ||
<!--T:3--> | |||
The first agent of the class – [[sitagliptin]] – was approved by the [[U.S. Food and Drug Administration|FDA]] in 2006. | The first agent of the class – [[sitagliptin]] – was approved by the [[U.S. Food and Drug Administration|FDA]] in 2006. | ||
<!--T:4--> | |||
[[Glucagon]] increases [[blood glucose]] levels, and DPP-4 inhibitors reduce glucagon and blood glucose levels. The mechanism of DPP-4 inhibitors is to increase [[incretin]] levels ([[GLP-1]] and [[gastric inhibitory polypeptide|GIP]]), which inhibit [[glucagon]] release, which in turn increases [[insulin]] secretion, decreases gastric emptying, and decreases [[blood glucose]] levels. | [[Glucagon]] increases [[blood glucose]] levels, and DPP-4 inhibitors reduce glucagon and blood glucose levels. The mechanism of DPP-4 inhibitors is to increase [[incretin]] levels ([[GLP-1]] and [[gastric inhibitory polypeptide|GIP]]), which inhibit [[glucagon]] release, which in turn increases [[insulin]] secretion, decreases gastric emptying, and decreases [[blood glucose]] levels. | ||
<!--T:5--> | |||
A 2018 [[meta-analysis]] found no favorable effect of DPP-4 inhibitors on all-cause mortality, cardiovascular mortality, [[myocardial infarction]] or [[stroke]] in patients with type 2 diabetes. | A 2018 [[meta-analysis]] found no favorable effect of DPP-4 inhibitors on all-cause mortality, cardiovascular mortality, [[myocardial infarction]] or [[stroke]] in patients with type 2 diabetes. | ||
==Examples== | ==Examples== <!--T:6--> | ||
Drugs belonging to this class are: | Drugs belonging to this class are: | ||
* [[Sitagliptin]] (FDA approved 2006, marketed by [[Merck & Co.]] as [[Januvia]]) | * [[Sitagliptin]] (FDA approved 2006, marketed by [[Merck & Co.]] as [[Januvia]]) | ||
| Line 31: | Line 38: | ||
* [[Prusogliptin]] | * [[Prusogliptin]] | ||
<!--T:7--> | |||
Other chemicals which may inhibit DPP-4 include: | Other chemicals which may inhibit DPP-4 include: | ||
* [[Berberine]], an [[alkaloid]] found in plants of the genus ''[[Berberis]]'', inhibits dipeptidyl peptidase-4 which may at least partly explains its antihyperglycemic activity. | * [[Berberine]], an [[alkaloid]] found in plants of the genus ''[[Berberis]]'', inhibits dipeptidyl peptidase-4 which may at least partly explains its antihyperglycemic activity. | ||
==Adverse effects== | ==Adverse effects== <!--T:8--> | ||
In those already taking [[sulphonylurea]]s, there is an increased risk of [[hypoglycemia|low blood sugar]] when taking a medicine in the DPP-4 drug class. | In those already taking [[sulphonylurea]]s, there is an increased risk of [[hypoglycemia|low blood sugar]] when taking a medicine in the DPP-4 drug class. | ||
<!--T:9--> | |||
Adverse effects include nasopharyngitis, [[headache]], [[nausea]], [[heart failure]], hypersensitivity and skin reactions. | Adverse effects include nasopharyngitis, [[headache]], [[nausea]], [[heart failure]], hypersensitivity and skin reactions. | ||
<!--T:10--> | |||
The U.S. Food and Drug Administration (FDA) is warning that the type 2 diabetes medicines like [[sitagliptin]], [[saxagliptin]], [[linagliptin]], and [[alogliptin]] may cause joint pain that can be severe and disabling. FDA has added a new Warning and Precaution about this risk to the labels of all medicines in this drug class, called dipeptidyl peptidase-4 (DPP-4) inhibitors. However, studies assessing risk of rheumatoid arthritis among DPP-4 inhibitor users have been inconclusive. | The U.S. Food and Drug Administration (FDA) is warning that the type 2 diabetes medicines like [[sitagliptin]], [[saxagliptin]], [[linagliptin]], and [[alogliptin]] may cause joint pain that can be severe and disabling. FDA has added a new Warning and Precaution about this risk to the labels of all medicines in this drug class, called dipeptidyl peptidase-4 (DPP-4) inhibitors. However, studies assessing risk of rheumatoid arthritis among DPP-4 inhibitor users have been inconclusive. | ||
<!--T:11--> | |||
A 2014 review found increased risk of [[heart failure]] with saxagliptin and alogliptin, prompting the FDA in 2016 to add warnings to the relevant drug labels. | A 2014 review found increased risk of [[heart failure]] with saxagliptin and alogliptin, prompting the FDA in 2016 to add warnings to the relevant drug labels. | ||
<!--T:12--> | |||
A 2018 meta analysis showed that use of DPP-4 inhibitors was associated with a 58% increased risk of developing acute pancreatitis compared with placebo or no treatment. | A 2018 meta analysis showed that use of DPP-4 inhibitors was associated with a 58% increased risk of developing acute pancreatitis compared with placebo or no treatment. | ||
<!--T:13--> | |||
A 2018 observational study suggested an elevated risk of developing inflammatory bowel disease (specifically, ulcerative colitis), reaching a peak after three to four years of use and decreasing after more than four years of use. | A 2018 observational study suggested an elevated risk of developing inflammatory bowel disease (specifically, ulcerative colitis), reaching a peak after three to four years of use and decreasing after more than four years of use. | ||
<!--T:14--> | |||
A 2020 Cochrane systematic review did not find enough evidence of reduction of all-cause mortality, serious adverse events, cardiovascular mortality, non-fatal [[myocardial infarction]], non-fatal [[stroke]] or [[Chronic kidney disease|end-stage renal disease]] when comparing [[metformin]] monotherapy to dipeptidyl peptidase-4 inhibitors for the treatment of type 2 diabetes. | A 2020 Cochrane systematic review did not find enough evidence of reduction of all-cause mortality, serious adverse events, cardiovascular mortality, non-fatal [[myocardial infarction]], non-fatal [[stroke]] or [[Chronic kidney disease|end-stage renal disease]] when comparing [[metformin]] monotherapy to dipeptidyl peptidase-4 inhibitors for the treatment of type 2 diabetes. | ||
===Cancer=== | ===Cancer=== <!--T:15--> | ||
In response to a report of precancerous changes in the pancreases of rats and organ donors treated with the DPP-4 inhibitor sitagliptin, the United States FDA and the European Medicines Agency each undertook independent reviews of all clinical and preclinical data related to the possible association of DPP-4 inhibitors with pancreatic cancer. In a joint letter to the New England Journal of Medicine, the agencies stated that they had not yet reached a final conclusion regarding a possible causative relationship. | In response to a report of precancerous changes in the pancreases of rats and organ donors treated with the DPP-4 inhibitor sitagliptin, the United States FDA and the European Medicines Agency each undertook independent reviews of all clinical and preclinical data related to the possible association of DPP-4 inhibitors with pancreatic cancer. In a joint letter to the New England Journal of Medicine, the agencies stated that they had not yet reached a final conclusion regarding a possible causative relationship. | ||
<!--T:16--> | |||
A 2014 meta-analysis found no evidence for increased [[pancreatic cancer]] risk in people treated with DPP-4 inhibitors, but owing to the modest amount of data available, was not able to completely exclude possible risk. | A 2014 meta-analysis found no evidence for increased [[pancreatic cancer]] risk in people treated with DPP-4 inhibitors, but owing to the modest amount of data available, was not able to completely exclude possible risk. | ||
==Combination drugs== | ==Combination drugs== <!--T:17--> | ||
Some DPP-4 inhibitor drugs have received approval from the FDA to be used with [[metformin]] concomitantly with additive effect to increase the level of glucagon-like peptide 1 (GLP-1) which also decreases [[hepatic]] [[gluconeogenesis|glucose production]]. | Some DPP-4 inhibitor drugs have received approval from the FDA to be used with [[metformin]] concomitantly with additive effect to increase the level of glucagon-like peptide 1 (GLP-1) which also decreases [[hepatic]] [[gluconeogenesis|glucose production]]. | ||
== See also == | == See also == <!--T:18--> | ||
* [[Development of dipeptidyl peptidase-4 inhibitors]] | * [[Development of dipeptidyl peptidase-4 inhibitors]] | ||
<!--T:19--> | |||
{{Oral hypoglycemics}} | {{Oral hypoglycemics}} | ||
{{Enzyme inhibition}} | {{Enzyme inhibition}} | ||
<!--T:20--> | |||
{{二次利用|date=1 February 2024}} | {{二次利用|date=1 February 2024}} | ||
{{DEFAULTSORT:Dipeptidyl Peptidase-4 Inhibitor}} | {{DEFAULTSORT:Dipeptidyl Peptidase-4 Inhibitor}} | ||
[[Category:Dipeptidyl peptidase-4 inhibitors| ]] | [[Category:Dipeptidyl peptidase-4 inhibitors| ]] | ||
</translate> | |||
Latest revision as of 17:34, 12 March 2024
Inhibitors of dipeptidyl peptidase 4 (DPP-4 inhibitors or gliptins) are a class of oral hypoglycemics that block the enzyme dipeptidyl peptidase-4 (DPP-4). They can be used to treat diabetes mellitus type 2.
The first agent of the class – sitagliptin – was approved by the FDA in 2006.
Glucagon increases blood glucose levels, and DPP-4 inhibitors reduce glucagon and blood glucose levels. The mechanism of DPP-4 inhibitors is to increase incretin levels (GLP-1 and GIP), which inhibit glucagon release, which in turn increases insulin secretion, decreases gastric emptying, and decreases blood glucose levels.
A 2018 meta-analysis found no favorable effect of DPP-4 inhibitors on all-cause mortality, cardiovascular mortality, myocardial infarction or stroke in patients with type 2 diabetes.
Examples
Drugs belonging to this class are:
- Sitagliptin (FDA approved 2006, marketed by Merck & Co. as Januvia)
- Vildagliptin (EU approved 2007, marketed in the EU by Novartis as Galvus)
- Saxagliptin (FDA approved in 2009, marketed as Onglyza)
- Linagliptin (FDA approved in 2011, marketed as Tradjenta by Eli Lilly and Company and Boehringer Ingelheim)
- Gemigliptin (approved in Korea in 2012, marketed by LG Life Sciences) Marketed as Zemiglo
- Anagliptin (approved in Japan as Suiny in 2012, marketed by Sanwa Kagaku Kenkyusho Co., Ltd. and Kowa Company, Ltd.)
- Teneligliptin (approved in Japan as Tenelia in 2012)
- Alogliptin (FDA approved 2013 as Nesina/ Vipidia, marketed by Takeda Pharmaceutical Company)
- Trelagliptin (approved for use in Japan as Zafatek/ Wedica in 2015)
- Omarigliptin (MK-3102) (approved as Marizev in Japan in 2015, developed by Merck & Co.; research showed that omarigliptin can be used as once-weekly treatment and generally well tolerated throughout the base and extension studies)
- Evogliptin (approved as Suganon/ Evodine for use in South Korea)
- Gosogliptin (approved as Saterex for use in Russia)
- Dutogliptin (PHX- 1149 free base, being developed by Phenomix Corporation), Phase III
- Retagliptin (SP-2086), approved in China.
- Denagliptin
- Cofrogliptin (HSK- 7653, compound 2)
- Fotagliptin
- Prusogliptin
Other chemicals which may inhibit DPP-4 include:
- Berberine, an alkaloid found in plants of the genus Berberis, inhibits dipeptidyl peptidase-4 which may at least partly explains its antihyperglycemic activity.
Adverse effects
In those already taking sulphonylureas, there is an increased risk of low blood sugar when taking a medicine in the DPP-4 drug class.
Adverse effects include nasopharyngitis, headache, nausea, heart failure, hypersensitivity and skin reactions.
The U.S. Food and Drug Administration (FDA) is warning that the type 2 diabetes medicines like sitagliptin, saxagliptin, linagliptin, and alogliptin may cause joint pain that can be severe and disabling. FDA has added a new Warning and Precaution about this risk to the labels of all medicines in this drug class, called dipeptidyl peptidase-4 (DPP-4) inhibitors. However, studies assessing risk of rheumatoid arthritis among DPP-4 inhibitor users have been inconclusive.
A 2014 review found increased risk of heart failure with saxagliptin and alogliptin, prompting the FDA in 2016 to add warnings to the relevant drug labels.
A 2018 meta analysis showed that use of DPP-4 inhibitors was associated with a 58% increased risk of developing acute pancreatitis compared with placebo or no treatment.
A 2018 observational study suggested an elevated risk of developing inflammatory bowel disease (specifically, ulcerative colitis), reaching a peak after three to four years of use and decreasing after more than four years of use.
A 2020 Cochrane systematic review did not find enough evidence of reduction of all-cause mortality, serious adverse events, cardiovascular mortality, non-fatal myocardial infarction, non-fatal stroke or end-stage renal disease when comparing metformin monotherapy to dipeptidyl peptidase-4 inhibitors for the treatment of type 2 diabetes.
Cancer
In response to a report of precancerous changes in the pancreases of rats and organ donors treated with the DPP-4 inhibitor sitagliptin, the United States FDA and the European Medicines Agency each undertook independent reviews of all clinical and preclinical data related to the possible association of DPP-4 inhibitors with pancreatic cancer. In a joint letter to the New England Journal of Medicine, the agencies stated that they had not yet reached a final conclusion regarding a possible causative relationship.
A 2014 meta-analysis found no evidence for increased pancreatic cancer risk in people treated with DPP-4 inhibitors, but owing to the modest amount of data available, was not able to completely exclude possible risk.
Combination drugs
Some DPP-4 inhibitor drugs have received approval from the FDA to be used with metformin concomitantly with additive effect to increase the level of glucagon-like peptide 1 (GLP-1) which also decreases hepatic glucose production.
See also
| この記事は、クリエイティブ・コモンズ・表示・継承ライセンス3.0のもとで公表されたウィキペディアの項目Dipeptidyl peptidase-4 inhibitor(1 February 2024編集記事参照)を素材として二次利用しています。 Item:Q21466 |