診断
Medical diagnosis/ja

Medical diagnosis (abbreviated Dx, Dx, or Ds) is the process of determining which disease or condition explains a person's symptoms and signs. It is most often referred to as diagnosis with the medical context being implicit. The information required for diagnosis is typically collected from a history and physical examination of the person seeking medical care. Often, one or more diagnostic procedures, such as medical tests, are also done during the process. Sometimes posthumous diagnosis is considered a kind of medical diagnosis.
Diagnosis is often challenging because many signs and symptoms are nonspecific. For example, redness of the skin (erythema), by itself, is a sign of many disorders and thus does not tell the healthcare professional what is wrong. Thus differential diagnosis, in which several possible explanations are compared and contrasted, must be performed. This involves the correlation of various pieces of information followed by the recognition and differentiation of patterns. Occasionally the process is made easy by a sign or symptom (or a group of several) that is pathognomonic.
Diagnosis is a major component of the procedure of a doctor's visit. From the point of view of statistics, the diagnostic procedure involves classification tests.
Medical uses
A diagnosis, in the sense of diagnostic procedure, can be regarded as an attempt at classification of an individual's condition into separate and distinct categories that allow medical decisions about treatment and prognosis to be made. Subsequently, a diagnostic opinion is often described in terms of a disease or other condition. (In the case of a wrong diagnosis, however, the individual's actual disease or condition is not the same as the individual's diagnosis.)
A diagnostic procedure may be performed by various healthcare professionals such as a physician, physiotherapist, dentist, podiatrist, optometrist, nurse practitioner, healthcare scientist or physician assistant. This article uses diagnostician as any of these person categories.
A diagnostic procedure (as well as the opinion reached thereby) does not necessarily involve elucidation of the etiology of the diseases or conditions of interest, that is, what caused the disease or condition. Such elucidation can be useful to optimize treatment, further specify the prognosis or prevent recurrence of the disease or condition in the future.
The initial task is to detect a medical indication to perform a diagnostic procedure. Indications include:
- Detection of any deviation from what is known to be normal, such as can be described in terms of, for example, anatomy (the structure of the human body), physiology (how the body works), pathology (what can go wrong with the anatomy and physiology), psychology (thought and behavior) and human homeostasis (regarding mechanisms to keep body systems in balance). Knowledge of what is normal and measuring of the patient's current condition against those norms can assist in determining the patient's particular departure from homeostasis and the degree of departure, which in turn can assist in quantifying the indication for further diagnostic processing.
- A complaint expressed by a patient.
- The fact that a patient has sought a diagnostician can itself be an indication to perform a diagnostic procedure. For example, in a doctor's visit, the physician may already start performing a diagnostic procedure by watching the gait of the patient from the waiting room to the doctor's office even before she or he has started to present any complaints.
Even during an already ongoing diagnostic procedure, there can be an indication to perform another, separate, diagnostic procedure for another, potentially concomitant, disease or condition. This may occur as a result of an incidental finding of a sign unrelated to the parameter of interest, such as can occur in comprehensive tests such as radiological studies like magnetic resonance imaging or blood test panels that also include blood tests that are not relevant for the ongoing diagnosis.
Procedure
General components which are present in a diagnostic procedure in most of the various available methods include:
- Complementing the already given information with further data gathering, which may include questions of the medical history (potentially from other people close to the patient as well), physical examination and various diagnostic tests.
A diagnostic test is any kind of medical test performed to aid in the diagnosis or detection of disease. Diagnostic tests can also be used to provide prognostic information on people with established disease. - Processing of the answers, findings or other results. Consultations with other providers and specialists in the field may be sought.
There are a number of methods or techniques that can be used in a diagnostic procedure, including performing a differential diagnosis or following medical algorithms. In reality, a diagnostic procedure may involve components of multiple methods.
Differential diagnosis
The method of differential diagnosis is based on finding as many candidate diseases or conditions as possible that can possibly cause the signs or symptoms, followed by a process of elimination or at least of rendering the entries more or less probable by further medical tests and other processing, aiming to reach the point where only one candidate disease or condition remains as probable. The result may also remain a list of possible conditions, ranked in order of probability or severity. Such a list is often generated by computer-aided diagnosis systems.
The resultant diagnostic opinion by this method can be regarded more or less as a diagnosis of exclusion. Even if it does not result in a single probable disease or condition, it can at least rule out any imminently life-threatening conditions.
Unless the provider is certain of the condition present, further medical tests, such as medical imaging, are performed or scheduled in part to confirm or disprove the diagnosis but also to document the patient's status and keep the patient's medical history up to date.
If unexpected findings are made during this process, the initial hypothesis may be ruled out and the provider must then consider other hypotheses.
Pattern recognition
In a pattern recognition method the provider uses experience to recognize a pattern of clinical characteristics. It is mainly based on certain symptoms or signs being associated with certain diseases or conditions, not necessarily involving the more cognitive processing involved in a differential diagnosis.
This may be the primary method used in cases where diseases are "obvious", or the provider's experience may enable him or her to recognize the condition quickly. Theoretically, a certain pattern of signs or symptoms can be directly associated with a certain therapy, even without a definite decision regarding what is the actual disease, but such a compromise carries a substantial risk of missing a diagnosis which actually has a different therapy so it may be limited to cases where no diagnosis can be made.
Diagnostic criteria
The term diagnostic criteria designates the specific combination of signs and symptoms, and test results that the clinician uses to attempt to determine the correct diagnosis.
Some examples of diagnostic criteria, also known as clinical case definitions, are:
Clinical decision support system
Clinical decision support systems are interactive computer programs designed to assist health professionals with decision-making tasks. The clinician interacts with the software utilizing both the clinician's knowledge and the software to make a better analysis of the patients data than either human or software could make on their own. Typically the system makes suggestions for the clinician to look through and the clinician picks useful information and removes erroneous suggestions. Some programs attempt to do this by replacing the clinician, such as reading the output of a heart monitor. Such automated processes are usually deemed a "device" by the FDA and require regulatory approval. In contrast, clinical decision support systems that "support" but do not replace the clinician are deemed to be "Augmented Intelligence" if it meets the FDA criteria that (1) it reveals the underlying data, (2) reveals the underlying logic, and (3) leaves the clinician in charge to shape and make the decision.
Other diagnostic procedure methods
Other methods that can be used in performing a diagnostic procedure include:
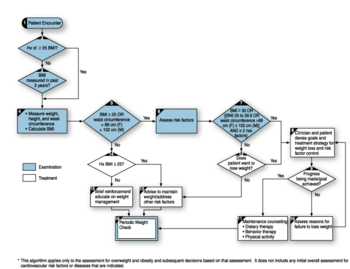
- Usage of medical algorithms
- An "exhaustive method", in which every possible question is asked and all possible data is collected.
Adverse effects
Diagnosis problems are the dominant cause of medical malpractice payments, accounting for 35% of total payments in a study of 25 years of data and 350,000 claims.
Overdiagnosis
Overdiagnosis is the diagnosis of "disease" that will never cause symptoms or death during a patient's lifetime. It is a problem because it turns people into patients unnecessarily and because it can lead to economic waste (overutilization) and treatments that may cause harm. Overdiagnosis occurs when a disease is diagnosed correctly, but the diagnosis is irrelevant. A correct diagnosis may be irrelevant because treatment for the disease is not available, not needed, or not wanted.
Errors
Most people will experience at least one diagnostic error in their lifetime, according to a 2015 report by the National Academies of Sciences, Engineering, and Medicine.
Causes and factors of error in diagnosis are:
- the manifestation of disease are not sufficiently noticeable
- a disease is omitted from consideration
- too much significance is given to some aspect of the diagnosis
- the condition is a rare disease with symptoms suggestive of many other conditions
- the condition has a rare presentation
Lag time
When making a medical diagnosis, a lag time is a delay in time until a step towards diagnosis of a disease or condition is made. Types of lag times are mainly:
- Onset-to-medical encounter lag time, the time from onset of symptoms until visiting a health care provider
- Encounter-to-diagnosis lag time, the time from first medical encounter to diagnosis
- Lag time due to delays in reading x-rays have been cited as a major challenge in care delivery. The Department of Health and Human Services has reportedly found that interpretation of x-rays is rarely available to emergency room physicians prior to patient discharge.
Long lag times are often called "diagnostic odyssey".
History
The first recorded examples of medical diagnosis are found in the writings of Imhotep (2630–2611 BC) in ancient Egypt (the Edwin Smith Papyrus). A Babylonian medical textbook, the Diagnostic Handbook written by Esagil-kin-apli (fl.1069–1046 BC), introduced the use of empiricism, logic and rationality in the diagnosis of an illness or disease. Traditional Chinese Medicine, as described in the Yellow Emperor's Inner Canon or Huangdi Neijing, specified four diagnostic methods: inspection, auscultation-olfaction, interrogation, and palpation. Hippocrates was known to make diagnoses by tasting his patients' urine and smelling their sweat.
Word
Medical diagnosis or the actual process of making a diagnosis is a cognitive process. A clinician uses several sources of data and puts the pieces of the puzzle together to make a diagnostic impression. The initial diagnostic impression can be a broad term describing a category of diseases instead of a specific disease or condition. After the initial diagnostic impression, the clinician obtains follow up tests and procedures to get more data to support or reject the original diagnosis and will attempt to narrow it down to a more specific level. Diagnostic procedures are the specific tools that the clinicians use to narrow the diagnostic possibilities.
The plural of diagnosis is diagnoses. The verb is to diagnose, and a person who diagnoses is called a diagnostician.
Etymology
The word diagnosis /daɪ.əɡˈnoʊsɪs/ is derived through Latin from the Greek word διάγνωσις (diágnōsis) from διαγιγνώσκειν (diagignṓskein), meaning "to discern, distinguish".
Society and culture
Social context
Diagnosis can take many forms. It might be a matter of naming the disease, lesion, dysfunction or disability. It might be a management-naming or prognosis-naming exercise. It may indicate either degree of abnormality on a continuum or kind of abnormality in a classification. It's influenced by non-medical factors such as power, ethics and financial incentives for patient or doctor. It can be a brief summation or an extensive formulation, even taking the form of a story or metaphor. It might be a means of communication such as a computer code through which it triggers payment, prescription, notification, information or advice. It might be pathogenic or salutogenic. It's generally uncertain and provisional.
Once a diagnostic opinion has been reached, the provider is able to propose a management plan, which will include treatment as well as plans for follow-up. From this point on, in addition to treating the patient's condition, the provider can educate the patient about the etiology, progression, prognosis, other outcomes, and possible treatments of her or his ailments, as well as providing advice for maintaining health.
A treatment plan is proposed which may include therapy and follow-up consultations and tests to monitor the condition and the progress of the treatment, if needed, usually according to the medical guidelines provided by the medical field on the treatment of the particular illness.
Relevant information should be added to the medical record of the patient.
A failure to respond to treatments that would normally work may indicate a need for review of the diagnosis.
Nancy McWilliams identifies five reasons that determine the necessity for diagnosis:
- diagnosis for treatment planning;
- information contained in it related to prognosis;
- protecting interests of patients;
- a diagnosis might help the therapist to empathize with his patient;
- might reduce the likelihood that some fearful patients will go-by the treatment.
種類
診断のサブタイプには以下のようなものがある:
- 臨床診断
- 診断テストではなく、医学的徴候や報告された症状に基づいてなされる診断。
- 検査室診断
- 患者の身体診察ではなく、検査室報告や検査結果に大きく基づく診断。例えば、感染症の適切な診断には、通常、徴候や症状の診察と、検査室での検査結果や関与する病原体の特徴の両方が必要である。
- 放射線診断
- 主に医用画像検査の結果に基づく診断。グリーンスティック骨折は一般的なX線診断である。
- 電気写真診断
- 電気生理学的活動の測定と記録に基づく診断である。
- 組織診断
- 生検や全臓器などの組織の巨視的、顕微鏡的、分子生物学的検査に基づく診断。例えば、がんの確定診断は、病理医による組織検査によって行われる。
- 主要診断
- 患者の主訴や医薬品の必要性に最も関連する単一の医学的診断。 多くの患者はさらに診断を追加している。
- 入院診断
- 患者が入院した理由としてつけられた診断名。実際の問題や、退院時に記録される診断名である退院診断とは異なる場合がある。
- 診断基準
- 臨床医が正しい診断を下すために用いる徴候、症状、検査結果の組み合わせを指す。通常、国際的な委員会によって発表される標準であり、最先端の技術を駆使して病態の存在を尊重し、可能な限り最高の感度と特異度を提供するように設計されている。
- 出生前診断
- 出生前に行われた診断作業
- 除外診断
- 病歴、診察、検査からその存在を完全に確信することができない医薬品。したがって診断は、他のすべての妥当な可能性を排除することによって行われる。
- 二重診断
- 関連はあるが別々の2つの病状または併存症の診断。この用語はほとんどの場合、重篤な精神疾患と物質使用障害の診断を指していたが、遺伝子検査の普及により、複数の遺伝性疾患を併発している患者の多くの症例が明らかになった。
- 自己診断
- 自分自身の病状を診断したり、特定したりすること。 自己診断は非常に一般的である。
- リモート診断
- 遠隔医療の一種で、患者と物理的に同じ部屋にいなくても診断ができる。
- 看護診断
- 看護診断は、生物学的なプロセスに焦点を当てるのではなく、変化への準備や援助を受け入れる意欲など、生活の状況に対する人々の反応を明らかにする。
- コンピューター支援診断
- 症状を提供することで、コンピュータは問題を特定し、その能力を最大限に発揮してユーザーを診断することができる。健康診断は症状がある身体の部位を特定することから始まり、コンピュータは対応する病気のデータベースを相互参照し、診断を提示する。
- 過剰診断
- 患者が生きている間に症状や苦痛、死亡を引き起こすことのない "病気 "と診断される。
- ゴミ箱診断
- 患者やカルテ部に貼られる曖昧な、あるいは完全に偽の、医学的あるいは精神医学的なレッテルであり、本質的に医学的でない理由、例えば、公式のように聞こえるレッテルを貼ることで患者を安心させるため、医療提供者を効果的に見せるため、あるいは治療の承認を得るためなどにつけられる。 この用語はまた、袋炎や老衰などの、議論のある、説明不足の、乱用された、または分類に疑問のある診断に対する蔑称として、あるいは、身体的空腹に対する正常な反応を反応性低血糖症とラベル付けするような、過剰医療化に相当する診断を退けるためのラベルとして使用される。
- 遡及的診断
- 歴史上の人物や特定の歴史上の出来事について、現代的な知識や方法、病気の分類を用いて病気をラベリングすること。
こちらも参照
- Diagnosis code/ja
- Diagnosis-related group/ja
- Diagnostic and Statistical Manual of Mental Disorders/ja
- 医師と患者の関係
- Etiology (medicine)/ja
- 疾病及び関連保健問題の
国際統計分類(ICD) - 医学的分類
- Merck Manual of Diagnosis and Therapy/ja
- Misdiagnosis/jaとmedical error/ja
- Nosology/ja
- Nursing diagnosis/ja
- Pathogenesis/ja
- Pathology/ja
- Prediction/ja
- Preimplantation genetic diagnosis/ja
- Prognosis/ja
- Sign (medicine)/ja
- Symptom/ja
リスト
外部リンク
- Media related to Medical diagnosis at Wikimedia Commons