カルシトリオール
Calcitriol/ja
カルシトリオールはビタミンDの活性型であり、通常は腎臓で作られる。別名1,25-ジヒドロキシコレカルシフェロールとも呼ばれる。カルシトリオールはホルモンであり、細胞核内のビタミンD受容体に結合して活性化し、多くの遺伝子の発現を増加させる。カルシトリオールは、主に腸からのカルシウムの取り込みを増加させることによって、血液中の生物におけるカルシウム(Ca2+)を増加させる。
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | US: /ˌkælsɪˈtraɪɒl/; UK: /kælˈsɪtriɒl/ |
| Trade names | Rocaltrol, Calcijex, Decostriol, others |
| Other names | 1,25-dihydroxycholecalciferol, 1alpha,25-dihydroxyvitamin D3, 1,25-dihydroxyvitamin D3, 1α,25-(OH)2D3, 1,25(OH)2D |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682335 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | 経口, intravenous/ja |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Protein binding | 99.9% |
| Metabolism | Kidney |
| Elimination half-life | 5~8時間(大人)、27時間(子供) |
| Excretion | 糞便(50%)、尿(16%) |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| PDB ligand | |
| Chemical and physical data | |
| Formula | C27H44O3 |
| Molar mass | 416.646 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
腎臓病による低血中カルシウム血症や副甲状腺機能亢進症、副甲状腺機能低下症による低血中カルシウム血症、骨粗鬆症、骨軟化症、家族性低リン血症の治療薬として投与され、経口または静脈への注射で服用できる。過剰量または過剰摂取は、脱力感、頭痛、吐き気、便秘、尿路感染症、腹痛を引き起こす可能性がある。重篤な副作用には、高血中カルシウムやアナフィラキシーがある。医薬品投与開始後および投与量変更時には、定期的な血液検査が推奨される。
カルシトリオールは1971年に活性型ビタミンDとして同定され、1978年に米国で医薬品として承認された。ジェネリック医薬品として販売されている。2021年には、1 万以上の処方で、米国で258番目に多く処方された医薬品であった。世界保健機関の必須医薬品リストに掲載されている。
Medical use
Calcitriol is prescribed for:
- Treatment of hypocalcaemia – hypoparathyroidism, osteomalacia (adults), rickets (infants, children), renal osteodystrophy, chronic kidney disease
- Treatment of osteoporosis
- Prevention of corticosteroid-induced osteoporosis
Calcitriol has been used in an ointment for the treatment of psoriasis, although the vitamin D analogue calcipotriol (calcipotriene) is more commonly used. Calcitriol has also been given by mouth for the treatment of psoriasis and psoriatic arthritis. Research on the noncalcemic actions of calcitriol and other VDR-ligand analogs and their possible therapeutic applications has been reviewed.
Adverse effects
The main adverse drug reaction associated with calcitriol therapy is hypercalcemia – early symptoms include: nausea, vomiting, constipation, anorexia, apathy, headache, thirst, pruritus, sweating, and/or polyuria. Compared to other vitamin D compounds in clinical use (cholecalciferol, ergocalciferol), calcitriol has a higher risk of inducing hypercalcemia. However, such episodes may be shorter and easier to treat due to its relatively short half-life.
High calcitriol levels may also be seen in human disease states in patients not on supplementation. In someone with hypercalcaemia and high calcitriol levels, low intact parathyroid hormone levels are usually present.
The major conditions with hypercalcaemia due to elevated calcitriol levels are lymphoma, tuberculosis and sarcoidosis where excess production occurs due to ectopic 25(OH)D-1-hydroxylase (CYP27B1) expressed in macrophages. Other conditions producing similar findings including:
- Fungal infections; Pneumocystis jiroveci, histoplasmosis, coccidioidomycosis, paracoccidioidomycosis, candidiasis
- Other granulomatous conditions; PR3+ vasculitis, Crohn's disease, acute granulomatous pneumonia, talc granuloma, silicone-induced granuloma, BCG-associated, granulomatous hepatitis, paraffin-associated granuloma
- Genetic conditions; Williams syndrome, pseudoxanthoma elasticum, CYP24A1 mutation (adult / infantile), SLC34A1 mutation
- Miscellaneous; mycobacterium avium, leprosy, lipoid pneumonia, cat scratch fever, berylliosis
Some plants contain glycosides of 1,25-dihydroxycholecalciferol. Consumption of these glycosides by grazing animals leads to vitamin D toxicity, resulting in calcinosis, the deposition of excessive calcium in soft tissues. Three rangeland plants, Cestrum diurnum, Solanum malacoxylon, and Trisetum flavescens are known to contain these glycosides. Of these, only C. diurnum is found in the U.S., mainly in Florida.
Mechanism of action
Calcitriol increases blood calcium levels ([Ca2+
]) by:
- Promoting absorption of dietary calcium from the gastrointestinal tract.
- Increasing renal tubular reabsorption of calcium, thus reducing the loss of calcium in the urine.
- Stimulating release of calcium from bone. For this it acts on the specific type of bone cells referred to as osteoblasts, causing them to release RANKL, which in turn activates osteoclasts.
Calcitriol acts in concert with parathyroid hormone (PTH) in all three of these roles. For instance, PTH also indirectly stimulates osteoclasts. However, the main effect of PTH is to increase the rate at which the kidneys excrete inorganic phosphate (Pi), the counterion of Ca2+
. The resulting decrease in serum phosphate causes hydroxyapatite (Ca5(PO4)3OH) to dissolve out of bone, thus increasing serum calcium. PTH also stimulates the production of calcitriol (see below).
Many of the effects of calcitriol are mediated by its interaction with the calcitriol receptor, also called the vitamin D receptor or VDR. For instance, the unbound inactive form of the calcitriol receptor in intestinal epithelial cells resides in the cytoplasm. When calcitriol binds to the receptor, the ligand-receptor complex translocates to the cell nucleus, where it acts as a transcription factor promoting the expression of a gene encoding a calcium binding protein. The levels of the calcium binding protein increase enabling the cells to actively transport more calcium (Ca2+
) from the intestine across the intestinal mucosa into the blood. Alternative, non-genomic pathways may be mediated through either PDIA3 or VDR.
The maintenance of electroneutrality requires that the transport of Ca2+
ions catalyzed by the intestinal epithelial cells be accompanied by counterions, primarily inorganic phosphate. Thus calcitriol also stimulates the intestinal absorption of phosphate.
The observation that calcitriol stimulates the release of calcium from bone seems contradictory, given that sufficient levels of serum calcitriol generally prevent overall loss of calcium from bone. It is believed that the increased levels of serum calcium resulting from calcitriol-stimulated intestinal uptake causes bone to take up more calcium than it loses by hormonal stimulation of osteoclasts. Only when there are conditions, such as dietary calcium deficiency or defects in intestinal transport, which result in a reduction of serum calcium does an overall loss of calcium from bone occur.
Calcitriol also inhibits the release of calcitonin, a hormone which reduces blood calcium primarily by inhibiting calcium release from bone.
Biosynthesis and its regulation

Calcitriol is produced in the cells of the proximal tubule of the nephron in the kidneys by the action of 25-hydroxyvitamin D3 1-alpha-hydroxylase, a mitochondrial oxygenase and an enzyme which catalyzes the hydroxylation of 25-hydroxycholecalciferol (calcifediol) in the 1-alpha position.
The activity of this enzyme is stimulated by PTH. This is an important control point in Ca2+ homeostasis. Additional effects on the production of calcitriol include an increase by prolactin, a hormone which stimulates lactogenesis (the formation of milk in mammary glands), a process which requires large amounts of calcium. Activity is also decreased by high levels of serum phosphate and by an increase in the production of the hormone FGF23 by osteocyte cells in bone.
Calcitriol is also produced outside the kidney in small amounts by many other tissues including placenta and activated macrophages.
When the drug alfacalcidol is used, 25-hydroxylation in the liver produces calcitriol as the active metabolite. This will produce greater effects than other vitamin D precursors in patients with kidney disease who have loss of the renal 1-alpha-hydroxylase.
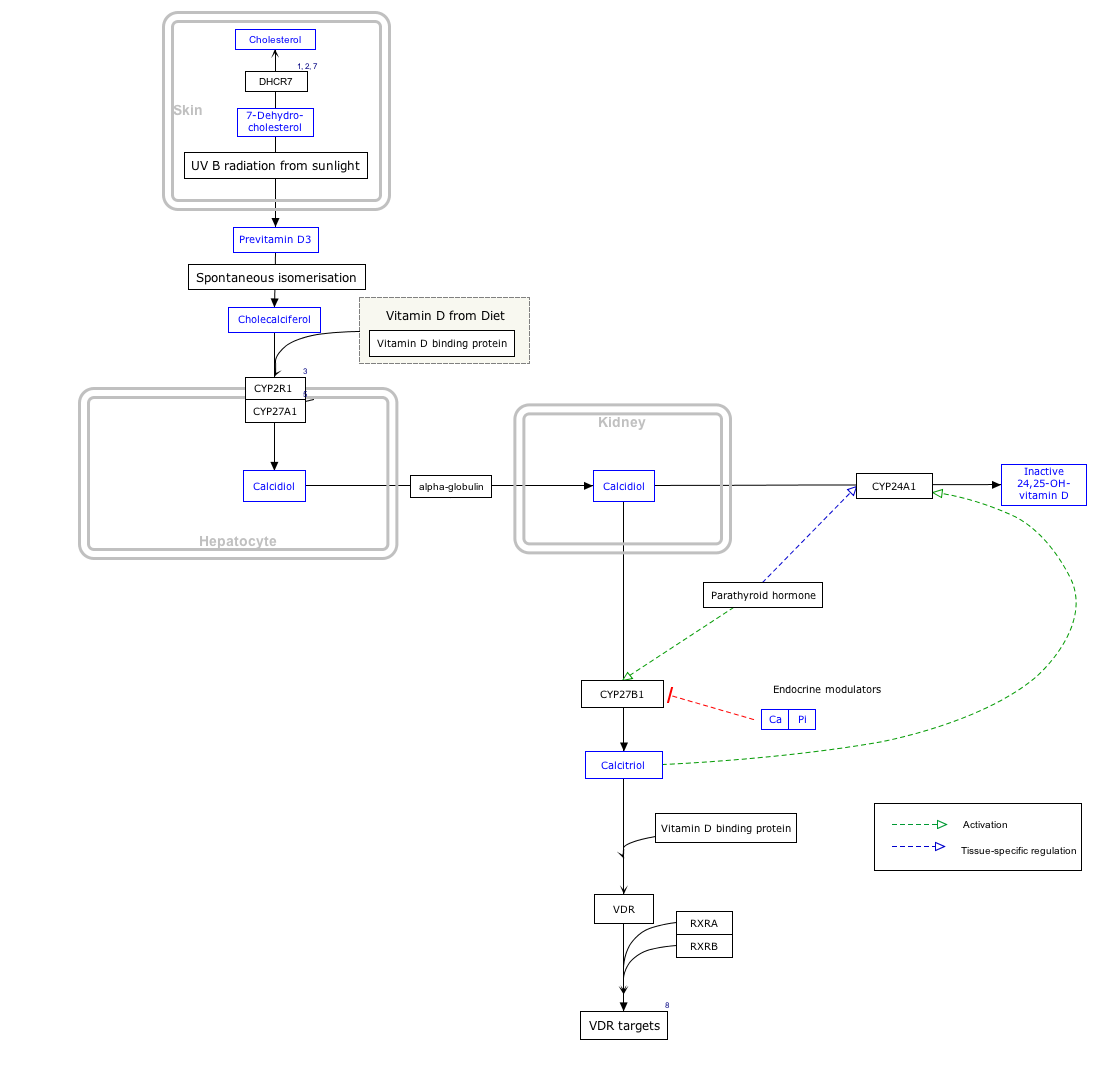
Interactive pathway map
Click on genes, proteins and metabolites below to link to respective articles. [§ 1]
- ↑ The interactive pathway map can be edited at WikiPathways: "VitaminDSynthesis_WP1531".
Metabolism
The halflife of calcitriol in the body is measured in hours, unlike its precursor calcifediol, whose halflife is measured in weeks. Calcitriol is inactivated by further hydroxylation to form 1,24,25-trihydroxyvitamin D, calcitroic acid. This occurs through the action of the CYP24A1 24-hydroxylase. Calcitroic acid is more soluble in water and is excreted in bile and urine.
History
It was first identified in 1971 by Michael F. Holick working in the laboratory of Hector DeLuca, and also by Tony Norman and colleagues.
名称
カルシトリオールは、特に1,25-ジヒドロキシコレカルシフェロールを指す。コレカルシフェロールはすでに1つのヒドロキシル基を持つため、この命名法ではさらに2つ(1,25)しか指定されないが、実際にはカルシトリオールという名称が示すように3つ(1,3,25-トリオール)存在する。1-ヒドロキシ基はα位にあり、これは例えば1α,25-(OH)2D3の略称のように名称に明記されることがある。
カルシトリオールは、厳密には、エルゴカルシフェロール(ビタミンD2)の水酸化生成物ではなく、コレカルシフェロール(ビタミンD3)に由来するカルシフェジオール(25-OHビタミンD3)の1-水酸化生成物である。1α,25-ジヒドロキシエルゴカルシフェロール(エルカルシトリオール)はビタミンD2産物に使用されるべきである。しかし、1,25-ジヒドロキシビタミンDまたは1,25(OH)2Dという用語は、両方の活性型ビタミンDを指すために使用されることが多い。実際、どちらもビタミンD受容体に結合し、生物学的効果をもたらす。
Calcitriol is marketed as a pharmaceutical for medical use under various trade names including Rocaltrol (Roche), Calcijex (Abbott), Decostriol (Mibe, Jesalis), Vectical (Galderma), and Rolsical (Sun Pharma).