Body mass index: Difference between revisions
No edit summary |
Marked this version for translation |
||
| Line 1: | Line 1: | ||
<languages /> | <languages /> | ||
<translate> | <translate> | ||
<!--T:1--> | |||
{{Short description|Relative weight based on mass and height}} | {{Short description|Relative weight based on mass and height}} | ||
{{Infobox diagnostic | {{Infobox diagnostic | ||
| Line 24: | Line 25: | ||
{{Human body weight}} | {{Human body weight}} | ||
<!--T:2--> | |||
'''Body mass index''' ('''BMI''') is a value derived from the [[mass]] ([[Mass versus weight|weight]]) and [[height]] of a person. The BMI is defined as the [[human body weight|body mass]] divided by the [[square (algebra)|square]] of the [[human height|body height]], and is expressed in [[Units of measurement|units]] of kg/m<sup>2</sup>, resulting from mass in [[kilogram]]s (kg) and height in [[metre]]s (m). | '''Body mass index''' ('''BMI''') is a value derived from the [[mass]] ([[Mass versus weight|weight]]) and [[height]] of a person. The BMI is defined as the [[human body weight|body mass]] divided by the [[square (algebra)|square]] of the [[human height|body height]], and is expressed in [[Units of measurement|units]] of kg/m<sup>2</sup>, resulting from mass in [[kilogram]]s (kg) and height in [[metre]]s (m). | ||
<!--T:3--> | |||
The BMI may be determined first by measuring its components by means of a [[weighing scale]] and a [[stadiometer]]. The multiplication and division may be carried out directly, by hand or using a calculator, or indirectly using a [[lookup table]] (or chart). The table displays BMI as a function of mass and height and may show other units of measurement (converted to [[Metric system|metric units]] for the calculation). The table may also show contour lines or colours for different BMI categories. | The BMI may be determined first by measuring its components by means of a [[weighing scale]] and a [[stadiometer]]. The multiplication and division may be carried out directly, by hand or using a calculator, or indirectly using a [[lookup table]] (or chart). The table displays BMI as a function of mass and height and may show other units of measurement (converted to [[Metric system|metric units]] for the calculation). The table may also show contour lines or colours for different BMI categories. | ||
<!--T:4--> | |||
The BMI is a convenient [[rule of thumb]] used to broadly categorize a person as based on tissue mass ([[muscle]], [[fat]], and [[bone]]) and height. Major adult BMI classifications are ''[[underweight]]'' (under 18.5 kg/m<sup>2</sup>), ''[[normal weight]]'' (18.5 to 24.9), ''[[overweight]]'' (25 to 29.9), and ''[[obese]]'' (30 or more). When used to predict an individual's health, rather than as a statistical measurement for groups, the BMI has [[#Limitations|limitations]] that can make it less useful than some of the [[#Alternatives|alternatives]], especially when applied to individuals with [[abdominal obesity]], [[short stature]], or [[Bodybuilding|high muscle mass]]. | The BMI is a convenient [[rule of thumb]] used to broadly categorize a person as based on tissue mass ([[muscle]], [[fat]], and [[bone]]) and height. Major adult BMI classifications are ''[[underweight]]'' (under 18.5 kg/m<sup>2</sup>), ''[[normal weight]]'' (18.5 to 24.9), ''[[overweight]]'' (25 to 29.9), and ''[[obese]]'' (30 or more). When used to predict an individual's health, rather than as a statistical measurement for groups, the BMI has [[#Limitations|limitations]] that can make it less useful than some of the [[#Alternatives|alternatives]], especially when applied to individuals with [[abdominal obesity]], [[short stature]], or [[Bodybuilding|high muscle mass]]. | ||
<!--T:5--> | |||
BMIs under 20 and over 25 have been associated with higher all-cause mortality, with the risk increasing with distance from the 20–25 range. | BMIs under 20 and over 25 have been associated with higher all-cause mortality, with the risk increasing with distance from the 20–25 range. | ||
{{TOC limit}} | {{TOC limit}} | ||
==History== | ==History== <!--T:6--> | ||
[[File:Obesity & BMI.png|thumb|Obesity and BMI]] | [[File:Obesity & BMI.png|thumb|Obesity and BMI]] | ||
[[Adolphe Quetelet]], a Belgian [[astronomer]], mathematician, [[statistician]], and [[sociologist]], devised the basis of the BMI between 1830 and 1850 as he developed what he called "social physics". Quetelet himself never intended for the index, then called the Quetelet Index, to be used as a means of medical assessment. Instead, it was a component of his study of {{lang|fr|l'homme moyen}}, or the average man. Quetelet thought of the average man as a social ideal, and developed the body mass index as a means of discovering the socially ideal human person. According to Lars Grue and Arvid Heiberg in the Scandinavian Journal of Disability Research, Quetelet's idealization of the average man would be elaborated upon by [[Francis Galton]] a decade later in the development of [[Eugenics]]. | [[Adolphe Quetelet]], a Belgian [[astronomer]], mathematician, [[statistician]], and [[sociologist]], devised the basis of the BMI between 1830 and 1850 as he developed what he called "social physics". Quetelet himself never intended for the index, then called the Quetelet Index, to be used as a means of medical assessment. Instead, it was a component of his study of {{lang|fr|l'homme moyen}}, or the average man. Quetelet thought of the average man as a social ideal, and developed the body mass index as a means of discovering the socially ideal human person. According to Lars Grue and Arvid Heiberg in the Scandinavian Journal of Disability Research, Quetelet's idealization of the average man would be elaborated upon by [[Francis Galton]] a decade later in the development of [[Eugenics]]. | ||
<!--T:7--> | |||
The modern term "body mass index" (BMI) for the ratio of [[human body weight]] to squared height was coined in a paper published in the July 1972 edition of the ''[[Journal of Chronic Diseases]]'' by [[Ancel Keys]] and others. In this paper, Keys argued that what he termed the BMI was "if not fully satisfactory, at least as good as any other relative weight index as an indicator of relative obesity". | The modern term "body mass index" (BMI) for the ratio of [[human body weight]] to squared height was coined in a paper published in the July 1972 edition of the ''[[Journal of Chronic Diseases]]'' by [[Ancel Keys]] and others. In this paper, Keys argued that what he termed the BMI was "if not fully satisfactory, at least as good as any other relative weight index as an indicator of relative obesity". | ||
<!--T:8--> | |||
The interest in an index that measures [[body fat]] came with observed increasing obesity in prosperous [[Western world|Western]] societies. Keys explicitly judged BMI as appropriate for ''population'' studies and inappropriate for individual evaluation. Nevertheless, due to its simplicity, it has come to be widely used for preliminary diagnoses. Additional metrics, such as waist circumference, can be more useful. | The interest in an index that measures [[body fat]] came with observed increasing obesity in prosperous [[Western world|Western]] societies. Keys explicitly judged BMI as appropriate for ''population'' studies and inappropriate for individual evaluation. Nevertheless, due to its simplicity, it has come to be widely used for preliminary diagnoses. Additional metrics, such as waist circumference, can be more useful. | ||
<!--T:9--> | |||
The BMI is expressed in kg/m<sup>2</sup>, resulting from mass in kilograms and height in metres. If [[Pound (mass)|pounds]] and [[inch]]es are used, a conversion factor of 703 (kg/m<sup>2</sup>)/(lb/in<sup>2</sup>) is applied. (If pounds and feet are used, a conversion factor of 4.88 is used.) When the term BMI is used informally, the units are usually omitted. | The BMI is expressed in kg/m<sup>2</sup>, resulting from mass in kilograms and height in metres. If [[Pound (mass)|pounds]] and [[inch]]es are used, a conversion factor of 703 (kg/m<sup>2</sup>)/(lb/in<sup>2</sup>) is applied. (If pounds and feet are used, a conversion factor of 4.88 is used.) When the term BMI is used informally, the units are usually omitted. | ||
<!--T:10--> | |||
:<math>\mathrm{BMI} = \frac{\text{mass}_\text{kg}}{{\text{height}_\text{m}}^2} | :<math>\mathrm{BMI} = \frac{\text{mass}_\text{kg}}{{\text{height}_\text{m}}^2} | ||
= \frac{\text{mass}_\text{lb}}{{\text{height}_\text{in}}^2}\times 703</math> | = \frac{\text{mass}_\text{lb}}{{\text{height}_\text{in}}^2}\times 703</math> | ||
<!--T:11--> | |||
BMI provides a simple numeric measure of a person's ''thickness'' or ''thinness'', allowing health professionals to discuss weight problems more objectively with their patients. BMI was designed to be used as a simple means of classifying average sedentary (physically inactive) populations, with an average [[body composition]]. For such individuals, the BMI value recommendations {{as of | 2014 | lc = on}} are as follows: 18.5 to 24.9 kg/m<sup>2</sup> may indicate optimal weight, lower than 18.5 may indicate [[underweight]], 25 to 29.9 may indicate [[overweight]], and 30 or more may indicate [[obesity|obese]]. Lean male athletes often have a high muscle-to-fat ratio and therefore a BMI that is misleadingly high relative to their body-fat percentage. | BMI provides a simple numeric measure of a person's ''thickness'' or ''thinness'', allowing health professionals to discuss weight problems more objectively with their patients. BMI was designed to be used as a simple means of classifying average sedentary (physically inactive) populations, with an average [[body composition]]. For such individuals, the BMI value recommendations {{as of | 2014 | lc = on}} are as follows: 18.5 to 24.9 kg/m<sup>2</sup> may indicate optimal weight, lower than 18.5 may indicate [[underweight]], 25 to 29.9 may indicate [[overweight]], and 30 or more may indicate [[obesity|obese]]. Lean male athletes often have a high muscle-to-fat ratio and therefore a BMI that is misleadingly high relative to their body-fat percentage. | ||
==Categories== | ==Categories== <!--T:12--> | ||
A common use of the BMI is to assess how far an individual's body weight departs from what is normal for a person's height. The weight excess or deficiency may, in part, be accounted for by body fat ([[adipose tissue]]) although other factors such as muscularity also affect BMI significantly (see discussion below and [[overweight]]). | A common use of the BMI is to assess how far an individual's body weight departs from what is normal for a person's height. The weight excess or deficiency may, in part, be accounted for by body fat ([[adipose tissue]]) although other factors such as muscularity also affect BMI significantly (see discussion below and [[overweight]]). | ||
<!--T:13--> | |||
The [[World Health Organization|WHO]] regards an adult BMI of less than 18.5 as underweight and possibly indicative of [[malnutrition]], an [[eating disorder]], or other health problems, while a BMI of 25 or more is considered overweight and 30 or more is considered [[obesity|obese]]. In addition to the principle, international WHO BMI cut-off points (16, 17, 18.5, 25, 30, 35 and 40), four additional cut-off points for at-risk Asians were identified (23, 27.5, 32.5 and 37.5). These ranges of BMI values are valid only as statistical categories. | The [[World Health Organization|WHO]] regards an adult BMI of less than 18.5 as underweight and possibly indicative of [[malnutrition]], an [[eating disorder]], or other health problems, while a BMI of 25 or more is considered overweight and 30 or more is considered [[obesity|obese]]. In addition to the principle, international WHO BMI cut-off points (16, 17, 18.5, 25, 30, 35 and 40), four additional cut-off points for at-risk Asians were identified (23, 27.5, 32.5 and 37.5). These ranges of BMI values are valid only as statistical categories. | ||
<!--T:14--> | |||
{| class="wikitable plainrowheaders" style="text-align:center" | {| class="wikitable plainrowheaders" style="text-align:center" | ||
|+ BMI, basic categories | |+ BMI, basic categories | ||
| Line 93: | Line 105: | ||
|} | |} | ||
===Children and youth=== | ===Children and youth=== <!--T:15--> | ||
[[File:BMIBoys 1.svg|thumb|BMI for age percentiles for boys 2 to 20 years of age]] | [[File:BMIBoys 1.svg|thumb|BMI for age percentiles for boys 2 to 20 years of age]] | ||
[[File:BMIGirls 1.svg|thumb|BMI for age percentiles for girls 2 to 20 years of age]] | [[File:BMIGirls 1.svg|thumb|BMI for age percentiles for girls 2 to 20 years of age]] | ||
BMI is used differently for people aged 2 to 20. It is calculated in the same way as for adults but then compared to typical values for other children or youth of the same age. Instead of comparison against fixed thresholds for underweight and overweight, the BMI is compared against the [[percentile]]s for children of the same sex and age. | BMI is used differently for people aged 2 to 20. It is calculated in the same way as for adults but then compared to typical values for other children or youth of the same age. Instead of comparison against fixed thresholds for underweight and overweight, the BMI is compared against the [[percentile]]s for children of the same sex and age. | ||
<!--T:16--> | |||
A BMI that is less than the 5th percentile is considered underweight and above the 95th percentile is considered obese. Children with a BMI between the 85th and 95th percentile are considered to be overweight. | A BMI that is less than the 5th percentile is considered underweight and above the 95th percentile is considered obese. Children with a BMI between the 85th and 95th percentile are considered to be overweight. | ||
Studies in Britain from 2013 have indicated that females between the ages 12 and 16 had a higher BMI than males of the same age by 1.0 kg/m<sup>2</sup> on average. | Studies in Britain from 2013 have indicated that females between the ages 12 and 16 had a higher BMI than males of the same age by 1.0 kg/m<sup>2</sup> on average. | ||
===International variations=== | ===International variations=== <!--T:17--> | ||
These recommended distinctions along the linear scale may vary from time to time and country to country, making global, longitudinal surveys problematic. People from different populations and descent have different associations between BMI, percentage of body fat, and health risks, with a higher risk of [[type 2 diabetes mellitus]] and [[Atherosclerosis|atherosclerotic]] cardiovascular disease at BMIs lower than the [[World Health Organization|WHO]] cut-off point for overweight, 25 kg/m<sup>2</sup>, although the cut-off for observed risk varies among different populations. The cut-off for observed risk varies based on populations and subpopulations in Europe, Asia and Africa. | These recommended distinctions along the linear scale may vary from time to time and country to country, making global, longitudinal surveys problematic. People from different populations and descent have different associations between BMI, percentage of body fat, and health risks, with a higher risk of [[type 2 diabetes mellitus]] and [[Atherosclerosis|atherosclerotic]] cardiovascular disease at BMIs lower than the [[World Health Organization|WHO]] cut-off point for overweight, 25 kg/m<sup>2</sup>, although the cut-off for observed risk varies among different populations. The cut-off for observed risk varies based on populations and subpopulations in Europe, Asia and Africa. | ||
====Hong Kong==== | ====Hong Kong==== <!--T:18--> | ||
The [[Hospital Authority]] of [[Hong Kong]] recommends the use of the following BMI ranges: | The [[Hospital Authority]] of [[Hong Kong]] recommends the use of the following BMI ranges: | ||
<!--T:19--> | |||
{| class="wikitable plainrowheaders" style="text-align:center" | {| class="wikitable plainrowheaders" style="text-align:center" | ||
|+ BMI in Hong Kong | |+ BMI in Hong Kong | ||
| Line 129: | Line 143: | ||
|} | |} | ||
====Japan==== | ====Japan==== <!--T:20--> | ||
A 2000 study from the Japan Society for the Study of Obesity (JASSO) presents the following table of BMI categories: | A 2000 study from the Japan Society for the Study of Obesity (JASSO) presents the following table of BMI categories: | ||
<!--T:21--> | |||
{| class="wikitable plainrowheaders" style="text-align:center" | {| class="wikitable plainrowheaders" style="text-align:center" | ||
|+ BMI in Japan | |+ BMI in Japan | ||
| Line 157: | Line 172: | ||
|} | |} | ||
====Singapore==== | ====Singapore==== <!--T:22--> | ||
In Singapore, the BMI cut-off figures were revised in 2005 by the Health Promotion Board (HPB), motivated by studies showing that many Asian populations, including Singaporeans, have a higher proportion of body fat and increased risk for cardiovascular diseases and [[diabetes mellitus]], compared with general BMI recommendations in other countries. The BMI cut-offs are presented with an emphasis on health risk rather than weight. | In Singapore, the BMI cut-off figures were revised in 2005 by the Health Promotion Board (HPB), motivated by studies showing that many Asian populations, including Singaporeans, have a higher proportion of body fat and increased risk for cardiovascular diseases and [[diabetes mellitus]], compared with general BMI recommendations in other countries. The BMI cut-offs are presented with an emphasis on health risk rather than weight. | ||
<!--T:23--> | |||
{| class="wikitable plainrowheaders" | {| class="wikitable plainrowheaders" | ||
|+ BMI in Singapore | |+ BMI in Singapore | ||
| Line 184: | Line 200: | ||
|} | |} | ||
==== United Kingdom ==== | ==== United Kingdom ==== <!--T:24--> | ||
In the UK, [[National Institute for Health and Care Excellence|NICE]] guidance recommends prevention of type 2 diabetes should start at a BMI of 30 in White and 27.5 in [[Black British people|Black African]], [[British African-Caribbean people|African-Caribbean]], [[South Asians in the United Kingdom|South Asian]], and [[British Chinese|Chinese]] populations. | In the UK, [[National Institute for Health and Care Excellence|NICE]] guidance recommends prevention of type 2 diabetes should start at a BMI of 30 in White and 27.5 in [[Black British people|Black African]], [[British African-Caribbean people|African-Caribbean]], [[South Asians in the United Kingdom|South Asian]], and [[British Chinese|Chinese]] populations. | ||
<!--T:25--> | |||
New research based on a large sample of almost 1.5 million people in England found that some ethnic groups would benefit from prevention at or above a BMI of (rounded): | New research based on a large sample of almost 1.5 million people in England found that some ethnic groups would benefit from prevention at or above a BMI of (rounded): | ||
* 30 in White | * 30 in White | ||
| Line 200: | Line 217: | ||
** 21 in [[British Bangladeshis|Bangladeshi]] | ** 21 in [[British Bangladeshis|Bangladeshi]] | ||
====United States==== | ====United States==== <!--T:26--> | ||
In 1998, the U.S. [[National Institutes of Health]] brought U.S. definitions in line with [[World Health Organization]] guidelines, lowering the normal/overweight cut-off from a BMI of 27.8 (men) and 27.3 (women) to a BMI of 25. This had the effect of redefining approximately 25 million Americans, previously ''healthy'', to ''overweight''. | In 1998, the U.S. [[National Institutes of Health]] brought U.S. definitions in line with [[World Health Organization]] guidelines, lowering the normal/overweight cut-off from a BMI of 27.8 (men) and 27.3 (women) to a BMI of 25. This had the effect of redefining approximately 25 million Americans, previously ''healthy'', to ''overweight''. | ||
<!--T:27--> | |||
This can partially explain the increase in the ''overweight'' diagnosis in the past 20 years, and the increase in sales of weight loss products during the same time. [[World Health Organization|WHO]] also recommends lowering the normal/overweight threshold for southeast Asian body types to around BMI 23, and expects further revisions to emerge from clinical studies of different body types. | This can partially explain the increase in the ''overweight'' diagnosis in the past 20 years, and the increase in sales of weight loss products during the same time. [[World Health Organization|WHO]] also recommends lowering the normal/overweight threshold for southeast Asian body types to around BMI 23, and expects further revisions to emerge from clinical studies of different body types. | ||
<!--T:28--> | |||
A survey in 2007 showed 63% of Americans were then overweight or obese, with 26% in the obese category (a BMI of 30 or more). By 2014, 37.7% of adults in the United States were obese, 35.0% of men and 40.4% of women; class 3 obesity (BMI over 40) values were 7.7% for men and 9.9% for women. The U.S. National Health and Nutrition Examination Survey of 2015-2016 showed that 71.6% of American men and women had BMIs over 25. Obesity—a BMI of 30 or more—was found in 39.8% of the US adults. | A survey in 2007 showed 63% of Americans were then overweight or obese, with 26% in the obese category (a BMI of 30 or more). By 2014, 37.7% of adults in the United States were obese, 35.0% of men and 40.4% of women; class 3 obesity (BMI over 40) values were 7.7% for men and 9.9% for women. The U.S. National Health and Nutrition Examination Survey of 2015-2016 showed that 71.6% of American men and women had BMIs over 25. Obesity—a BMI of 30 or more—was found in 39.8% of the US adults. | ||
<!--T:29--> | |||
<div> | <div> | ||
{| class="wikitable plainrowheaders floatleft" | {| class="wikitable plainrowheaders floatleft" | ||
| Line 314: | Line 334: | ||
|} | |} | ||
<!--T:30--> | |||
{| class="wikitable plainrowheaders" | {| class="wikitable plainrowheaders" | ||
|- | |- | ||
| Line 422: | Line 443: | ||
</div> | </div> | ||
==Consequences of elevated level in adults== | ==Consequences of elevated level in adults== <!--T:31--> | ||
The BMI ranges are based on the relationship between body weight and disease and death. Overweight and obese individuals are at an increased risk for the following diseases: | The BMI ranges are based on the relationship between body weight and disease and death. Overweight and obese individuals are at an increased risk for the following diseases: | ||
* [[Coronary artery disease]] | * [[Coronary artery disease]] | ||
| Line 436: | Line 457: | ||
* Epidural [[lipomatosis]] | * Epidural [[lipomatosis]] | ||
<!--T:32--> | |||
Among people who have never smoked, overweight/obesity is associated with 51% increase in mortality compared with people who have always been a normal weight. | Among people who have never smoked, overweight/obesity is associated with 51% increase in mortality compared with people who have always been a normal weight. | ||
==Applications== | ==Applications== <!--T:33--> | ||
===Public health=== | ===Public health=== <!--T:34--> | ||
The BMI is generally used as a means of correlation between groups related by general mass and can serve as a vague means of estimating [[adipose tissue|adiposity]]. The duality of the BMI is that, while it is easy to use as a general calculation, it is limited as to how accurate and pertinent the data obtained from it can be. Generally, the index is suitable for recognizing trends within sedentary or overweight individuals because there is a smaller margin of error. The BMI has been used by the [[World Health Organization|WHO]] as the standard for recording obesity statistics since the early 1980s. | The BMI is generally used as a means of correlation between groups related by general mass and can serve as a vague means of estimating [[adipose tissue|adiposity]]. The duality of the BMI is that, while it is easy to use as a general calculation, it is limited as to how accurate and pertinent the data obtained from it can be. Generally, the index is suitable for recognizing trends within sedentary or overweight individuals because there is a smaller margin of error. The BMI has been used by the [[World Health Organization|WHO]] as the standard for recording obesity statistics since the early 1980s. | ||
<!--T:35--> | |||
This general correlation is particularly useful for consensus data regarding obesity or various other conditions because it can be used to build a semi-accurate representation from which a solution can be stipulated, or the [[Recommended Dietary Allowance|RDA]] for a group can be calculated. Similarly, this is becoming more and more pertinent to the growth of children, since the majority of children are sedentary. | This general correlation is particularly useful for consensus data regarding obesity or various other conditions because it can be used to build a semi-accurate representation from which a solution can be stipulated, or the [[Recommended Dietary Allowance|RDA]] for a group can be calculated. Similarly, this is becoming more and more pertinent to the growth of children, since the majority of children are sedentary. | ||
Cross-sectional studies indicated that sedentary people can decrease BMI by becoming more physically active. Smaller effects are seen in prospective cohort studies which lend to support [[active mobility]] as a means to prevent a further increase in BMI. | Cross-sectional studies indicated that sedentary people can decrease BMI by becoming more physically active. Smaller effects are seen in prospective cohort studies which lend to support [[active mobility]] as a means to prevent a further increase in BMI. | ||
===Legislation=== | ===Legislation=== <!--T:36--> | ||
In France, Italy, and Spain, legislation has been introduced banning the usage of fashion show models having a BMI below 18. In Israel, a model with BMI below 18.5 is banned. This is done to fight [[Anorexia nervosa|anorexia]] among models and people interested in fashion. | In France, Italy, and Spain, legislation has been introduced banning the usage of fashion show models having a BMI below 18. In Israel, a model with BMI below 18.5 is banned. This is done to fight [[Anorexia nervosa|anorexia]] among models and people interested in fashion. | ||
==Relationship to health== | ==Relationship to health== <!--T:37--> | ||
A study published by ''[[Journal of the American Medical Association]]'' (''JAMA'') in 2005 showed that ''overweight'' people had a death rate similar to ''normal'' weight people as defined by BMI, while ''underweight'' and ''obese'' people had a higher death rate. | A study published by ''[[Journal of the American Medical Association]]'' (''JAMA'') in 2005 showed that ''overweight'' people had a death rate similar to ''normal'' weight people as defined by BMI, while ''underweight'' and ''obese'' people had a higher death rate. | ||
<!--T:38--> | |||
A study published by ''[[The Lancet]]'' in 2009 involving 900,000 adults showed that ''overweight'' and ''underweight'' people both had a mortality rate higher than ''normal'' weight people as defined by BMI. The optimal BMI was found to be in the range of 22.5–25. The average BMI of athletes is 22.4 for women and 23.6 for men. | A study published by ''[[The Lancet]]'' in 2009 involving 900,000 adults showed that ''overweight'' and ''underweight'' people both had a mortality rate higher than ''normal'' weight people as defined by BMI. The optimal BMI was found to be in the range of 22.5–25. The average BMI of athletes is 22.4 for women and 23.6 for men. | ||
<!--T:39--> | |||
High BMI is associated with [[diabetes mellitus type 2|type 2 diabetes]] only in people with high serum [[gamma-glutamyl transpeptidase]]. | High BMI is associated with [[diabetes mellitus type 2|type 2 diabetes]] only in people with high serum [[gamma-glutamyl transpeptidase]]. | ||
<!--T:40--> | |||
In an analysis of 40 studies involving 250,000 people, patients with coronary artery disease with ''normal'' BMIs were at higher risk of death from cardiovascular disease than people whose BMIs put them in the ''overweight'' range (BMI 25–29.9). | In an analysis of 40 studies involving 250,000 people, patients with coronary artery disease with ''normal'' BMIs were at higher risk of death from cardiovascular disease than people whose BMIs put them in the ''overweight'' range (BMI 25–29.9). | ||
<!--T:41--> | |||
One study found that BMI had a good general correlation with body fat percentage, and noted that obesity has overtaken smoking as the world's number one cause of death. But it also notes that in the study 50% of men and 62% of women were obese according to body fat defined obesity, while only 21% of men and 31% of women were obese according to BMI, meaning that BMI was found to underestimate the number of obese subjects. | One study found that BMI had a good general correlation with body fat percentage, and noted that obesity has overtaken smoking as the world's number one cause of death. But it also notes that in the study 50% of men and 62% of women were obese according to body fat defined obesity, while only 21% of men and 31% of women were obese according to BMI, meaning that BMI was found to underestimate the number of obese subjects. | ||
<!--T:42--> | |||
A 2010 study that followed 11,000 subjects for up to eight years concluded that BMI is not the most appropriate measure for the risk of heart attack, stroke or death. A better measure was found to be the [[waist-to-height ratio]]. A 2011 study that followed 60,000 participants for up to 13 years found that [[waist–hip ratio]] was a better predictor of ischaemic heart disease mortality. | A 2010 study that followed 11,000 subjects for up to eight years concluded that BMI is not the most appropriate measure for the risk of heart attack, stroke or death. A better measure was found to be the [[waist-to-height ratio]]. A 2011 study that followed 60,000 participants for up to 13 years found that [[waist–hip ratio]] was a better predictor of ischaemic heart disease mortality. | ||
==Limitations== | ==Limitations== <!--T:43--> | ||
[[File:Correlation between BMI and Percent Body Fat for Men in NCHS' NHANES 1994 Data.PNG|right|395px|thumb|This graph shows the correlation between body mass index (BMI) and body fat percentage (BFP) for 8550 men in [[National Center for Health Statistics|NCHS]]' [[National Health and Nutrition Examination Survey|NHANES]] 1994 data. Data in the upper left and lower right quadrants suggest the limitations of BMI.]] | [[File:Correlation between BMI and Percent Body Fat for Men in NCHS' NHANES 1994 Data.PNG|right|395px|thumb|This graph shows the correlation between body mass index (BMI) and body fat percentage (BFP) for 8550 men in [[National Center for Health Statistics|NCHS]]' [[National Health and Nutrition Examination Survey|NHANES]] 1994 data. Data in the upper left and lower right quadrants suggest the limitations of BMI.]] | ||
The medical establishment and statistical community have both highlighted the limitations of BMI. | The medical establishment and statistical community have both highlighted the limitations of BMI. | ||
=== Racial and gender differences === | === Racial and gender differences === <!--T:44--> | ||
Part of the statistical limitations of the BMI scale is the result of Quetelet's original sampling methods. As noted in his primary work, A Treatise on Man and the Development of His Faculties, the data from which Quetelet derived his formula was taken mostly from Scottish Highland soldiers and French [[Gendarmerie]]. The BMI was always designed as a metric for European men. For women, and people of non-European origin, the scale is often biased. As noted by sociologist Sabrina Strings, the BMI is largely inaccurate for black people especially, disproportionately labelling them as overweight even for healthy individuals. | Part of the statistical limitations of the BMI scale is the result of Quetelet's original sampling methods. As noted in his primary work, A Treatise on Man and the Development of His Faculties, the data from which Quetelet derived his formula was taken mostly from Scottish Highland soldiers and French [[Gendarmerie]]. The BMI was always designed as a metric for European men. For women, and people of non-European origin, the scale is often biased. As noted by sociologist Sabrina Strings, the BMI is largely inaccurate for black people especially, disproportionately labelling them as overweight even for healthy individuals. | ||
===Scaling=== | ===Scaling=== <!--T:45--> | ||
The exponent in the denominator of the formula for BMI is arbitrary. The BMI depends upon weight and the ''square'' of height. Since mass increases to the ''third power'' of linear dimensions, taller individuals with exactly the same body shape and relative composition have a larger BMI. BMI is proportional to the mass and inversely proportional to the square of the height. So, if all body dimensions double, and mass scales naturally with the cube of the height, then BMI doubles instead of remaining the same. This results in taller people having a reported BMI that is uncharacteristically high, compared to their actual body fat levels. In comparison, the [[Ponderal index]] is based on the natural scaling of mass with the third power of the height. | The exponent in the denominator of the formula for BMI is arbitrary. The BMI depends upon weight and the ''square'' of height. Since mass increases to the ''third power'' of linear dimensions, taller individuals with exactly the same body shape and relative composition have a larger BMI. BMI is proportional to the mass and inversely proportional to the square of the height. So, if all body dimensions double, and mass scales naturally with the cube of the height, then BMI doubles instead of remaining the same. This results in taller people having a reported BMI that is uncharacteristically high, compared to their actual body fat levels. In comparison, the [[Ponderal index]] is based on the natural scaling of mass with the third power of the height. | ||
<!--T:46--> | |||
However, many taller people are not just "scaled up" short people but tend to have narrower frames in proportion to their height. [[Carl Lavie]] has written that "The B.M.I. tables are excellent for identifying obesity and body fat in large populations, but they are far less reliable for determining fatness in individuals." | However, many taller people are not just "scaled up" short people but tend to have narrower frames in proportion to their height. [[Carl Lavie]] has written that "The B.M.I. tables are excellent for identifying obesity and body fat in large populations, but they are far less reliable for determining fatness in individuals." | ||
<!--T:47--> | |||
For US adults, exponent estimates range from 1.92 to 1.96 for males and from 1.45 to 1.95 for females. | For US adults, exponent estimates range from 1.92 to 1.96 for males and from 1.45 to 1.95 for females. | ||
===Physical characteristics=== | ===Physical characteristics=== <!--T:48--> | ||
The BMI overestimates roughly 10% for a large (or tall) frame and underestimates roughly 10% for a smaller frame (short stature). In other words, people with small frames would be carrying more fat than optimal, but their BMI indicates that they are ''normal''. Conversely, large framed (or tall) individuals may be quite healthy, with a fairly low [[body fat percentage]], but be classified as ''overweight'' by BMI. | The BMI overestimates roughly 10% for a large (or tall) frame and underestimates roughly 10% for a smaller frame (short stature). In other words, people with small frames would be carrying more fat than optimal, but their BMI indicates that they are ''normal''. Conversely, large framed (or tall) individuals may be quite healthy, with a fairly low [[body fat percentage]], but be classified as ''overweight'' by BMI. | ||
<!--T:49--> | |||
For example, a height/weight chart may say the ideal weight (BMI 21.5) for a {{convert|5|ft|10|in|m|order=flip|adj=mid|-tall}} man is {{convert|150|lb|kg|order=flip}}. But if that man has a slender build (small frame), he may be overweight at {{cvt|150|lb|kg|disp=or|order=flip}} and should reduce by 10% to roughly {{cvt|135|lb|kg|disp=or|order=flip}} (BMI 19.4). In the reverse, the man with a larger frame and more solid build should increase by 10%, to roughly {{cvt|165|lb|kg|disp=or|order=flip}} (BMI 23.7). If one teeters on the edge of small/medium or medium/large, common sense should be used in calculating one's ideal weight. However, falling into one's ideal weight range for height and build is still not as accurate in determining health risk factors as [[waist-to-height ratio]] and actual body fat percentage. | For example, a height/weight chart may say the ideal weight (BMI 21.5) for a {{convert|5|ft|10|in|m|order=flip|adj=mid|-tall}} man is {{convert|150|lb|kg|order=flip}}. But if that man has a slender build (small frame), he may be overweight at {{cvt|150|lb|kg|disp=or|order=flip}} and should reduce by 10% to roughly {{cvt|135|lb|kg|disp=or|order=flip}} (BMI 19.4). In the reverse, the man with a larger frame and more solid build should increase by 10%, to roughly {{cvt|165|lb|kg|disp=or|order=flip}} (BMI 23.7). If one teeters on the edge of small/medium or medium/large, common sense should be used in calculating one's ideal weight. However, falling into one's ideal weight range for height and build is still not as accurate in determining health risk factors as [[waist-to-height ratio]] and actual body fat percentage. | ||
<!--T:50--> | |||
Accurate frame size calculators use several measurements (wrist circumference, elbow width, neck circumference, and others) to determine what category an individual falls into for a given height. The BMI also fails to take into account loss of height through ageing. In this situation, BMI will increase without any corresponding increase in weight. | Accurate frame size calculators use several measurements (wrist circumference, elbow width, neck circumference, and others) to determine what category an individual falls into for a given height. The BMI also fails to take into account loss of height through ageing. In this situation, BMI will increase without any corresponding increase in weight. | ||
===Muscle versus fat=== | ===Muscle versus fat=== <!--T:51--> | ||
Assumptions about the distribution between muscle mass and fat mass are inexact. BMI generally overestimates [[adipose tissue|adiposity]] on those with leaner body mass (e.g., athletes) and underestimates excess adiposity on those with fattier body mass. | Assumptions about the distribution between muscle mass and fat mass are inexact. BMI generally overestimates [[adipose tissue|adiposity]] on those with leaner body mass (e.g., athletes) and underestimates excess adiposity on those with fattier body mass. | ||
<!--T:52--> | |||
A study in June 2008 by Romero-Corral et al. examined 13,601 subjects from the United States' third [[National Health and Nutrition Examination Survey]] (NHANES III) and found that BMI-defined obesity (BMI ≥ 30) was present in 21% of men and 31% of women. Body fat-defined obesity was found in 50% of men and 62% of women. While BMI-defined obesity showed high [[Sensitivity and specificity|specificity]] (95% for men and 99% for women), BMI showed poor [[Sensitivity and specificity|sensitivity]] (36% for men and 49% for women). In other words, the BMI will be mostly correct when determining a person to be obese, but can err quite frequently when determining a person not to be. Despite this undercounting of obesity by BMI, BMI values in the intermediate BMI range of 20–30 were found to be associated with a wide range of body fat percentages. For men with a BMI of 25, about 20% have a body fat percentage below 20% and about 10% have body fat percentage above 30%. | A study in June 2008 by Romero-Corral et al. examined 13,601 subjects from the United States' third [[National Health and Nutrition Examination Survey]] (NHANES III) and found that BMI-defined obesity (BMI ≥ 30) was present in 21% of men and 31% of women. Body fat-defined obesity was found in 50% of men and 62% of women. While BMI-defined obesity showed high [[Sensitivity and specificity|specificity]] (95% for men and 99% for women), BMI showed poor [[Sensitivity and specificity|sensitivity]] (36% for men and 49% for women). In other words, the BMI will be mostly correct when determining a person to be obese, but can err quite frequently when determining a person not to be. Despite this undercounting of obesity by BMI, BMI values in the intermediate BMI range of 20–30 were found to be associated with a wide range of body fat percentages. For men with a BMI of 25, about 20% have a body fat percentage below 20% and about 10% have body fat percentage above 30%. | ||
<!--T:53--> | |||
Body composition for athletes is often better calculated using measures of body fat, as determined by such techniques as skinfold measurements or underwater weighing and the limitations of manual measurement have also led to new, alternative methods to measure obesity, such as the [[Classification of obesity#Body Volume Index|body volume indicator]]. | Body composition for athletes is often better calculated using measures of body fat, as determined by such techniques as skinfold measurements or underwater weighing and the limitations of manual measurement have also led to new, alternative methods to measure obesity, such as the [[Classification of obesity#Body Volume Index|body volume indicator]]. | ||
===Variation in definitions of categories=== | ===Variation in definitions of categories=== <!--T:54--> | ||
It is not clear where on the BMI scale the threshold for ''[[overweight]]'' and ''[[obesity|obese]]'' should be set. Because of this, the standards have varied over the past few decades. Between 1980 and 2000 the U.S. Dietary Guidelines have defined overweight at a variety of levels ranging from a BMI of 24.9 to 27.1. In 1985 the [[National Institutes of Health]] (NIH) consensus conference recommended that overweight BMI be set at a BMI of 27.8 for men and 27.3 for women. | It is not clear where on the BMI scale the threshold for ''[[overweight]]'' and ''[[obesity|obese]]'' should be set. Because of this, the standards have varied over the past few decades. Between 1980 and 2000 the U.S. Dietary Guidelines have defined overweight at a variety of levels ranging from a BMI of 24.9 to 27.1. In 1985 the [[National Institutes of Health]] (NIH) consensus conference recommended that overweight BMI be set at a BMI of 27.8 for men and 27.3 for women. | ||
<!--T:55--> | |||
In 1998, an NIH report concluded that a BMI over 25 is overweight and a BMI over 30 is obese. In the 1990s the [[World Health Organization]] (WHO) decided that a BMI of 25 to 30 should be considered overweight and a BMI over 30 is obese, the standards the NIH set. This became the definitive guide for determining if someone is overweight. | In 1998, an NIH report concluded that a BMI over 25 is overweight and a BMI over 30 is obese. In the 1990s the [[World Health Organization]] (WHO) decided that a BMI of 25 to 30 should be considered overweight and a BMI over 30 is obese, the standards the NIH set. This became the definitive guide for determining if someone is overweight. | ||
<!--T:56--> | |||
One study found that the vast majority of people labelled 'overweight' and 'obese' according to current definitions do not in fact face any meaningful increased risk for early death. In a quantitative analysis of several studies, involving more than 600,000 men and women, the lowest mortality rates were found for people with BMIs between 23 and 29; most of the 25–30 range considered 'overweight' was not associated with higher risk. | One study found that the vast majority of people labelled 'overweight' and 'obese' according to current definitions do not in fact face any meaningful increased risk for early death. In a quantitative analysis of several studies, involving more than 600,000 men and women, the lowest mortality rates were found for people with BMIs between 23 and 29; most of the 25–30 range considered 'overweight' was not associated with higher risk. | ||
==Alternatives== | ==Alternatives== <!--T:57--> | ||
===Corpulence index (exponent of 3)=== | ===Corpulence index (exponent of 3)=== <!--T:58--> | ||
The [[corpulence index]] uses an exponent of 3 rather than 2. The corpulence index yields valid results even for very short and very tall people, which is a problem with BMI. For example, a {{convert|152.4|cm|ftin|abbr=on}} tall person at an ideal body weight of {{convert|48|kg|lb|abbr=on}} gives a normal BMI of 20.74 and CI of 13.6, while a {{convert|200|cm|ftin|abbr=on}} tall person with a weight of {{convert|100|kg|lb|abbr=on}} gives a BMI of 24.84, very close to an overweight BMI of 25, and a CI of 12.4, very close to a normal CI of 12. | The [[corpulence index]] uses an exponent of 3 rather than 2. The corpulence index yields valid results even for very short and very tall people, which is a problem with BMI. For example, a {{convert|152.4|cm|ftin|abbr=on}} tall person at an ideal body weight of {{convert|48|kg|lb|abbr=on}} gives a normal BMI of 20.74 and CI of 13.6, while a {{convert|200|cm|ftin|abbr=on}} tall person with a weight of {{convert|100|kg|lb|abbr=on}} gives a BMI of 24.84, very close to an overweight BMI of 25, and a CI of 12.4, very close to a normal CI of 12. | ||
===New BMI (exponent of 2.5)=== | ===New BMI (exponent of 2.5)=== <!--T:59--> | ||
An exponent of 5/2 was proposed by Quetelet in the 19{{sup|th}} century: | An exponent of 5/2 was proposed by Quetelet in the 19{{sup|th}} century: | ||
<blockquote>In general, we do not err much when we assume that during development the squares of the weight at different ages are as the fifth powers of the height</blockquote> | <blockquote>In general, we do not err much when we assume that during development the squares of the weight at different ages are as the fifth powers of the height</blockquote> | ||
<!--T:60--> | |||
This exponent of 2.5 is used in a revised formula for Body Mass Index, proposed by [[Nick Trefethen]], Professor of numerical analysis at the [[University of Oxford]], which minimizes the distortions for shorter and taller individuals resulting from the use of an exponent of 2 in the traditional BMI formula: | This exponent of 2.5 is used in a revised formula for Body Mass Index, proposed by [[Nick Trefethen]], Professor of numerical analysis at the [[University of Oxford]], which minimizes the distortions for shorter and taller individuals resulting from the use of an exponent of 2 in the traditional BMI formula: | ||
:<math>\mathrm{BMI}_\text{new} = 1.3 \times \frac{\text{mass}_\text{kg}}{\text{height}_\text{m}^{2.5}}</math> | :<math>\mathrm{BMI}_\text{new} = 1.3 \times \frac{\text{mass}_\text{kg}}{\text{height}_\text{m}^{2.5}}</math> | ||
The scaling factor of 1.3 was determined to make the proposed new BMI formula align with the traditional BMI formula for adults of average height, while the exponent of 2.5 is a compromise between the exponent of 2 in the traditional formula for BMI and the exponent of 3 that would be expected for the scaling of weight (which at constant density would theoretically scale with volume, i.e., as the cube of the height) with height. In Trefethen's analysis, an exponent of 2.5 was found to fit empirical data more closely with less distortion than either an exponent of 2 or 3. | The scaling factor of 1.3 was determined to make the proposed new BMI formula align with the traditional BMI formula for adults of average height, while the exponent of 2.5 is a compromise between the exponent of 2 in the traditional formula for BMI and the exponent of 3 that would be expected for the scaling of weight (which at constant density would theoretically scale with volume, i.e., as the cube of the height) with height. In Trefethen's analysis, an exponent of 2.5 was found to fit empirical data more closely with less distortion than either an exponent of 2 or 3. | ||
===BMI prime (exponent of 2, normalization factor)=== | ===BMI prime (exponent of 2, normalization factor)=== <!--T:61--> | ||
BMI Prime, a modification of the BMI system, is the ratio of actual BMI to upper limit optimal BMI (currently defined at 25 kg/m<sup>2</sup>), i.e., the actual BMI expressed as a proportion of upper limit optimal. BMI Prime is a [[dimensionless number]] independent of units. Individuals with BMI Prime less than 0.74 are underweight; those with between 0.74 and 1.00 have optimal weight; and those at 1.00 or greater are overweight. BMI Prime is useful clinically because it shows by what ratio (e.g. 1.36) or percentage (e.g. 136%, or 36% above) a person deviates from the maximum optimal BMI. | BMI Prime, a modification of the BMI system, is the ratio of actual BMI to upper limit optimal BMI (currently defined at 25 kg/m<sup>2</sup>), i.e., the actual BMI expressed as a proportion of upper limit optimal. BMI Prime is a [[dimensionless number]] independent of units. Individuals with BMI Prime less than 0.74 are underweight; those with between 0.74 and 1.00 have optimal weight; and those at 1.00 or greater are overweight. BMI Prime is useful clinically because it shows by what ratio (e.g. 1.36) or percentage (e.g. 136%, or 36% above) a person deviates from the maximum optimal BMI. | ||
<!--T:62--> | |||
For instance, a person with BMI 34 kg/m<sup>2</sup> has a BMI Prime of 34/25 = 1.36, and is 36% over their upper mass limit. In South East Asian and South Chinese populations (see [[#International variations|§ international variations]]), BMI Prime should be calculated using an upper limit BMI of 23 in the denominator instead of 25. BMI Prime allows easy comparison between populations whose upper-limit optimal BMI values differ. | For instance, a person with BMI 34 kg/m<sup>2</sup> has a BMI Prime of 34/25 = 1.36, and is 36% over their upper mass limit. In South East Asian and South Chinese populations (see [[#International variations|§ international variations]]), BMI Prime should be calculated using an upper limit BMI of 23 in the denominator instead of 25. BMI Prime allows easy comparison between populations whose upper-limit optimal BMI values differ. | ||
===Waist circumference=== | ===Waist circumference=== <!--T:63--> | ||
{{Main|Waist-to-height ratio|Waist-to-hip ratio}} | {{Main|Waist-to-height ratio|Waist-to-hip ratio}} | ||
Waist circumference is a good indicator of [[visceral fat]], which poses more health risks than fat elsewhere. According to the U.S. [[National Institutes of Health]] (NIH), waist circumference in excess of {{cvt|1020|mm}} for men and {{cvt|880|mm}} for (non-pregnant) women is considered to imply a high risk for type 2 diabetes, [[dyslipidemia]], [[hypertension]], and [[cardiovascular disease]] CVD. Waist circumference can be a better indicator of obesity-related disease risk than BMI. For example, this is the case in populations of Asian descent and older people. {{cvt|940|mm}} for men and {{cvt|800|mm}} for women has been stated to pose "higher risk", with the NIH figures "even higher". | Waist circumference is a good indicator of [[visceral fat]], which poses more health risks than fat elsewhere. According to the U.S. [[National Institutes of Health]] (NIH), waist circumference in excess of {{cvt|1020|mm}} for men and {{cvt|880|mm}} for (non-pregnant) women is considered to imply a high risk for type 2 diabetes, [[dyslipidemia]], [[hypertension]], and [[cardiovascular disease]] CVD. Waist circumference can be a better indicator of obesity-related disease risk than BMI. For example, this is the case in populations of Asian descent and older people. {{cvt|940|mm}} for men and {{cvt|800|mm}} for women has been stated to pose "higher risk", with the NIH figures "even higher". | ||
<!--T:64--> | |||
Waist-to-hip circumference ratio has also been used, but has been found to be no better than waist circumference alone, and more complicated to measure. | Waist-to-hip circumference ratio has also been used, but has been found to be no better than waist circumference alone, and more complicated to measure. | ||
<!--T:65--> | |||
A related indicator is waist circumference divided by height. The values indicating increased risk are: greater than 0.5 for people under 40 years of age, 0.5 to 0.6 for people aged 40–50, and greater than 0.6 for people over 50 years of age. | A related indicator is waist circumference divided by height. The values indicating increased risk are: greater than 0.5 for people under 40 years of age, 0.5 to 0.6 for people aged 40–50, and greater than 0.6 for people over 50 years of age. | ||
=== Surface-based body shape index === | === Surface-based body shape index === <!--T:66--> | ||
The Surface-based Body Shape Index (SBSI) is far more rigorous and is based upon four key measurements: the [[body surface area]] (BSA), vertical trunk circumference (VTC), waist circumference (WC) and height (H). Data on 11,808 subjects from the National Health and Human Nutrition Examination Surveys (NHANES) 1999–2004, showed that SBSI outperformed BMI, waist circumference, and [[Body Shape Index|A Body Shape Index (ABSI)]], an alternative to BMI. | The Surface-based Body Shape Index (SBSI) is far more rigorous and is based upon four key measurements: the [[body surface area]] (BSA), vertical trunk circumference (VTC), waist circumference (WC) and height (H). Data on 11,808 subjects from the National Health and Human Nutrition Examination Surveys (NHANES) 1999–2004, showed that SBSI outperformed BMI, waist circumference, and [[Body Shape Index|A Body Shape Index (ABSI)]], an alternative to BMI. | ||
<!--T:67--> | |||
: <math>\mathrm{SBSI} = \frac{(\text{H}^{7/4})(\text{WC}^{5/6})}{\text{BSA VTC}}</math> | : <math>\mathrm{SBSI} = \frac{(\text{H}^{7/4})(\text{WC}^{5/6})}{\text{BSA VTC}}</math> | ||
<!--T:68--> | |||
A simplified, dimensionless form of SBSI, known as SBSI<sup>*</sup>, has also been developed. | A simplified, dimensionless form of SBSI, known as SBSI<sup>*</sup>, has also been developed. | ||
<!--T:69--> | |||
: <math>\mathrm{SBSI^\star} = \frac{(\text{H}^2)(\text{WC})}{\text{BSA VTC}}</math> | : <math>\mathrm{SBSI^\star} = \frac{(\text{H}^2)(\text{WC})}{\text{BSA VTC}}</math> | ||
===Modified body mass index=== | ===Modified body mass index=== <!--T:70--> | ||
Within some medical contexts, such as [[familial amyloid polyneuropathy]], serum albumin is factored in to produce a modified body mass index (mBMI). The mBMI can be obtained by multiplying the BMI by [[human serum albumin|serum albumin]], in grams per litre. | Within some medical contexts, such as [[familial amyloid polyneuropathy]], serum albumin is factored in to produce a modified body mass index (mBMI). The mBMI can be obtained by multiplying the BMI by [[human serum albumin|serum albumin]], in grams per litre. | ||
== See also == | == See also == <!--T:71--> | ||
<!-- Please keep entries in alphabetical order & add a short description per [[WP:SEEALSO]] --> | <!-- Please keep entries in alphabetical order & add a short description per [[WP:SEEALSO]] --> | ||
* [[Allometry]] | * [[Allometry]] | ||
| Line 546: | Line 589: | ||
<!-- please keep entries in alphabetical order --> | <!-- please keep entries in alphabetical order --> | ||
== Further reading == | == Further reading == <!--T:72--> | ||
{{Refbegin}} | {{Refbegin}} | ||
* {{Cite book | veditors = Ferrera LA |year=2006 |title=Focus on Body Mass Index And Health Research |location=New York |publisher=Nova Science |isbn=978-1-59454-963-2}} | * {{Cite book | veditors = Ferrera LA |year=2006 |title=Focus on Body Mass Index And Health Research |location=New York |publisher=Nova Science |isbn=978-1-59454-963-2}} | ||
| Line 553: | Line 596: | ||
{{Refend}} | {{Refend}} | ||
== External links == | == External links == <!--T:73--> | ||
{{Wiktionary|body mass index}} | {{Wiktionary|body mass index}} | ||
<!-- Please do not add more links to more calculators. If you feel a particular online calculator has specific merits, please propose the link on the talk page. --> | <!-- Please do not add more links to more calculators. If you feel a particular online calculator has specific merits, please propose the link on the talk page. --> | ||
| Line 560: | Line 603: | ||
** {{Cite web | url = https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/english_bmi_calculator/bmi_calculator.html | title = BMI calculator ages 20 and older | date = 21 July 2021 | publisher = US Centers for Disease Control and Prevention }} | ** {{Cite web | url = https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/english_bmi_calculator/bmi_calculator.html | title = BMI calculator ages 20 and older | date = 21 July 2021 | publisher = US Centers for Disease Control and Prevention }} | ||
<!--T:74--> | |||
{{二次利用|date=26 February 2024}} | {{二次利用|date=26 February 2024}} | ||
{{DEFAULTSORT:Body Mass Index}} | {{DEFAULTSORT:Body Mass Index}} | ||
Latest revision as of 20:16, 28 February 2024
| Body mass index (BMI) | |
|---|---|
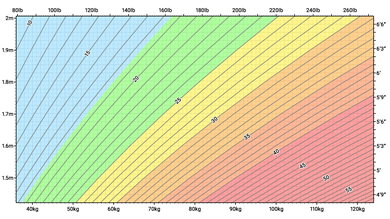 Chart showing body mass index (BMI) for a range of heights and weights in both metric and imperial. Colours indicate BMI categories defined by the World Health Organization; underweight, normal weight, overweight, moderately obese, severely obese and very severely obese. | |
| Synonyms | Quetelet index |
| MeSH | D015992 |
| MedlinePlus | 007196 |
| LOINC | 39156-5 |
| Part of a series on |
| Human body weight |
|---|
Body mass index (BMI) is a value derived from the mass (weight) and height of a person. The BMI is defined as the body mass divided by the square of the body height, and is expressed in units of kg/m2, resulting from mass in kilograms (kg) and height in metres (m).
The BMI may be determined first by measuring its components by means of a weighing scale and a stadiometer. The multiplication and division may be carried out directly, by hand or using a calculator, or indirectly using a lookup table (or chart). The table displays BMI as a function of mass and height and may show other units of measurement (converted to metric units for the calculation). The table may also show contour lines or colours for different BMI categories.
The BMI is a convenient rule of thumb used to broadly categorize a person as based on tissue mass (muscle, fat, and bone) and height. Major adult BMI classifications are underweight (under 18.5 kg/m2), normal weight (18.5 to 24.9), overweight (25 to 29.9), and obese (30 or more). When used to predict an individual's health, rather than as a statistical measurement for groups, the BMI has limitations that can make it less useful than some of the alternatives, especially when applied to individuals with abdominal obesity, short stature, or high muscle mass.
BMIs under 20 and over 25 have been associated with higher all-cause mortality, with the risk increasing with distance from the 20–25 range.
History

Adolphe Quetelet, a Belgian astronomer, mathematician, statistician, and sociologist, devised the basis of the BMI between 1830 and 1850 as he developed what he called "social physics". Quetelet himself never intended for the index, then called the Quetelet Index, to be used as a means of medical assessment. Instead, it was a component of his study of l'homme moyen, or the average man. Quetelet thought of the average man as a social ideal, and developed the body mass index as a means of discovering the socially ideal human person. According to Lars Grue and Arvid Heiberg in the Scandinavian Journal of Disability Research, Quetelet's idealization of the average man would be elaborated upon by Francis Galton a decade later in the development of Eugenics.
The modern term "body mass index" (BMI) for the ratio of human body weight to squared height was coined in a paper published in the July 1972 edition of the Journal of Chronic Diseases by Ancel Keys and others. In this paper, Keys argued that what he termed the BMI was "if not fully satisfactory, at least as good as any other relative weight index as an indicator of relative obesity".
The interest in an index that measures body fat came with observed increasing obesity in prosperous Western societies. Keys explicitly judged BMI as appropriate for population studies and inappropriate for individual evaluation. Nevertheless, due to its simplicity, it has come to be widely used for preliminary diagnoses. Additional metrics, such as waist circumference, can be more useful.
The BMI is expressed in kg/m2, resulting from mass in kilograms and height in metres. If pounds and inches are used, a conversion factor of 703 (kg/m2)/(lb/in2) is applied. (If pounds and feet are used, a conversion factor of 4.88 is used.) When the term BMI is used informally, the units are usually omitted.
BMI provides a simple numeric measure of a person's thickness or thinness, allowing health professionals to discuss weight problems more objectively with their patients. BMI was designed to be used as a simple means of classifying average sedentary (physically inactive) populations, with an average body composition. For such individuals, the BMI value recommendations 2014 年現在[update] are as follows: 18.5 to 24.9 kg/m2 may indicate optimal weight, lower than 18.5 may indicate underweight, 25 to 29.9 may indicate overweight, and 30 or more may indicate obese. Lean male athletes often have a high muscle-to-fat ratio and therefore a BMI that is misleadingly high relative to their body-fat percentage.
Categories
A common use of the BMI is to assess how far an individual's body weight departs from what is normal for a person's height. The weight excess or deficiency may, in part, be accounted for by body fat (adipose tissue) although other factors such as muscularity also affect BMI significantly (see discussion below and overweight).
The WHO regards an adult BMI of less than 18.5 as underweight and possibly indicative of malnutrition, an eating disorder, or other health problems, while a BMI of 25 or more is considered overweight and 30 or more is considered obese. In addition to the principle, international WHO BMI cut-off points (16, 17, 18.5, 25, 30, 35 and 40), four additional cut-off points for at-risk Asians were identified (23, 27.5, 32.5 and 37.5). These ranges of BMI values are valid only as statistical categories.
| Category | BMI (kg/m2) | BMI Prime |
|---|---|---|
| Underweight (Severe thinness) | < 16.0 | < 0.64 |
| Underweight (Moderate thinness) | 16.0 – 16.9 | 0.64 – 0.67 |
| Underweight (Mild thinness) | 17.0 – 18.4 | 0.68 – 0.73 |
| Normal range | 18.5 – 24.9 | 0.74 – 0.99 |
| Overweight (Pre-obese) | 25.0 – 29.9 | 1.00 – 1.19 |
| Obese (Class I) | 30.0 – 34.9 | 1.20 – 1.39 |
| Obese (Class II) | 35.0 – 39.9 | 1.40 – 1.59 |
| Obese (Class III) | ≥ 40.0 | ≥ 1.60 |
Children and youth
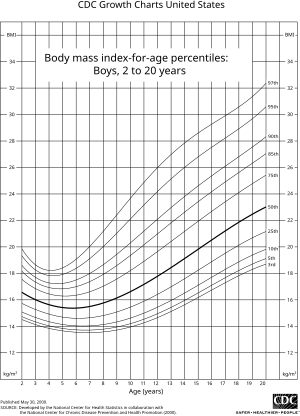

BMI is used differently for people aged 2 to 20. It is calculated in the same way as for adults but then compared to typical values for other children or youth of the same age. Instead of comparison against fixed thresholds for underweight and overweight, the BMI is compared against the percentiles for children of the same sex and age.
A BMI that is less than the 5th percentile is considered underweight and above the 95th percentile is considered obese. Children with a BMI between the 85th and 95th percentile are considered to be overweight. Studies in Britain from 2013 have indicated that females between the ages 12 and 16 had a higher BMI than males of the same age by 1.0 kg/m2 on average.
International variations
These recommended distinctions along the linear scale may vary from time to time and country to country, making global, longitudinal surveys problematic. People from different populations and descent have different associations between BMI, percentage of body fat, and health risks, with a higher risk of type 2 diabetes mellitus and atherosclerotic cardiovascular disease at BMIs lower than the WHO cut-off point for overweight, 25 kg/m2, although the cut-off for observed risk varies among different populations. The cut-off for observed risk varies based on populations and subpopulations in Europe, Asia and Africa.
Hong Kong
The Hospital Authority of Hong Kong recommends the use of the following BMI ranges:
| Category | BMI (kg/m2) |
|---|---|
| Underweight (Unhealthy) | < 18.5 |
| Normal range (Healthy) | 18.5 – 22.9 |
| Overweight I (At risk) | 23.0 – 24.9 |
| Overweight II (Moderately obese) | 25.0 – 29.9 |
| Overweight III (Severely obese) | ≥ 30.0 |
Japan
A 2000 study from the Japan Society for the Study of Obesity (JASSO) presents the following table of BMI categories:
| Category | BMI (kg/m2) |
|---|---|
| Underweight (Thin) | < 18.5 |
| Normal weight | 18.5 – 24.9 |
| Obesity (Class 1) | 25.0 – 29.9 |
| Obesity (Class 2) | 30.0 – 34.9 |
| Obesity (Class 3) | 35.0 – 39.9 |
| Obesity (Class 4) | ≥ 40.0 |
Singapore
In Singapore, the BMI cut-off figures were revised in 2005 by the Health Promotion Board (HPB), motivated by studies showing that many Asian populations, including Singaporeans, have a higher proportion of body fat and increased risk for cardiovascular diseases and diabetes mellitus, compared with general BMI recommendations in other countries. The BMI cut-offs are presented with an emphasis on health risk rather than weight.
| Category | BMI (kg/m2) | Health risk |
|---|---|---|
| Underweight | < 18.5 | Possible nutritional deficiency and osteoporosis. |
| Normal | 18.5 – 22.9 | Low risk (healthy range). |
| Mild to moderate overweight | 23.0 – 27.4 | Moderate risk of developing heart disease, high blood pressure, stroke, diabetes mellitus. |
| Very overweight to obese | ≥ 27.5 | High risk of developing heart disease, high blood pressure, stroke, diabetes mellitus. Metabolic Syndrome. |
United Kingdom
In the UK, NICE guidance recommends prevention of type 2 diabetes should start at a BMI of 30 in White and 27.5 in Black African, African-Caribbean, South Asian, and Chinese populations.
New research based on a large sample of almost 1.5 million people in England found that some ethnic groups would benefit from prevention at or above a BMI of (rounded):
- 30 in White
- 28 in Black
- just below 30 in Black British
- 29 in Black African
- 27 in Black Other
- 26 in Black Caribbean
- 27 in Arab and Chinese
- 24 in South Asian
- 24 in Pakistani, Indian and Nepali
- 23 in Tamil and Sri Lankan
- 21 in Bangladeshi
United States
In 1998, the U.S. National Institutes of Health brought U.S. definitions in line with World Health Organization guidelines, lowering the normal/overweight cut-off from a BMI of 27.8 (men) and 27.3 (women) to a BMI of 25. This had the effect of redefining approximately 25 million Americans, previously healthy, to overweight.
This can partially explain the increase in the overweight diagnosis in the past 20 years, and the increase in sales of weight loss products during the same time. WHO also recommends lowering the normal/overweight threshold for southeast Asian body types to around BMI 23, and expects further revisions to emerge from clinical studies of different body types.
A survey in 2007 showed 63% of Americans were then overweight or obese, with 26% in the obese category (a BMI of 30 or more). By 2014, 37.7% of adults in the United States were obese, 35.0% of men and 40.4% of women; class 3 obesity (BMI over 40) values were 7.7% for men and 9.9% for women. The U.S. National Health and Nutrition Examination Survey of 2015-2016 showed that 71.6% of American men and women had BMIs over 25. Obesity—a BMI of 30 or more—was found in 39.8% of the US adults.
| Age | Percentile | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 5th | 10th | 15th | 25th | 50th | 75th | 85th | 90th | 95th | |
| ≥ 20 (total) | 20.7 | 22.2 | 23.0 | 24.6 | 27.7 | 31.6 | 34.0 | 36.1 | 39.8 |
| 20–29 | 19.3 | 20.5 | 21.2 | 22.5 | 25.5 | 30.5 | 33.1 | 35.1 | 39.2 |
| 30–39 | 21.1 | 22.4 | 23.3 | 24.8 | 27.5 | 31.9 | 35.1 | 36.5 | 39.3 |
| 40–49 | 21.9 | 23.4 | 24.3 | 25.7 | 28.5 | 31.9 | 34.4 | 36.5 | 40.0 |
| 50–59 | 21.6 | 22.7 | 23.6 | 25.4 | 28.3 | 32.0 | 34.0 | 35.2 | 40.3 |
| 60–69 | 21.6 | 22.7 | 23.6 | 25.3 | 28.0 | 32.4 | 35.3 | 36.9 | 41.2 |
| 70–79 | 21.5 | 23.2 | 23.9 | 25.4 | 27.8 | 30.9 | 33.1 | 34.9 | 38.9 |
| ≥ 80 | 20.0 | 21.5 | 22.5 | 24.1 | 26.3 | 29.0 | 31.1 | 32.3 | 33.8 |
| Age | Percentile | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 5th | 10th | 15th | 25th | 50th | 75th | 85th | 90th | 95th | |
| ≥ 20 (total) | 19.6 | 21.0 | 22.0 | 23.6 | 27.7 | 33.2 | 36.5 | 39.3 | 43.3 |
| 20–29 | 18.6 | 19.8 | 20.7 | 21.9 | 25.6 | 31.8 | 36.0 | 38.9 | 42.0 |
| 30–39 | 19.8 | 21.1 | 22.0 | 23.3 | 27.6 | 33.1 | 36.6 | 40.0 | 44.7 |
| 40–49 | 20.0 | 21.5 | 22.5 | 23.7 | 28.1 | 33.4 | 37.0 | 39.6 | 44.5 |
| 50–59 | 19.9 | 21.5 | 22.2 | 24.5 | 28.6 | 34.4 | 38.3 | 40.7 | 45.2 |
| 60–69 | 20.0 | 21.7 | 23.0 | 24.5 | 28.9 | 33.4 | 36.1 | 38.7 | 41.8 |
| 70–79 | 20.5 | 22.1 | 22.9 | 24.6 | 28.3 | 33.4 | 36.5 | 39.1 | 42.9 |
| ≥ 80 | 19.3 | 20.4 | 21.3 | 23.3 | 26.1 | 29.7 | 30.9 | 32.8 | 35.2 |
Consequences of elevated level in adults
The BMI ranges are based on the relationship between body weight and disease and death. Overweight and obese individuals are at an increased risk for the following diseases:
- Coronary artery disease
- Dyslipidemia
- Type 2 diabetes
- Gallbladder disease
- Hypertension
- Osteoarthritis
- Sleep apnea
- Stroke
- Infertility
- At least 10 cancers, including endometrial, breast, and colon cancer
- Epidural lipomatosis
Among people who have never smoked, overweight/obesity is associated with 51% increase in mortality compared with people who have always been a normal weight.
Applications
Public health
The BMI is generally used as a means of correlation between groups related by general mass and can serve as a vague means of estimating adiposity. The duality of the BMI is that, while it is easy to use as a general calculation, it is limited as to how accurate and pertinent the data obtained from it can be. Generally, the index is suitable for recognizing trends within sedentary or overweight individuals because there is a smaller margin of error. The BMI has been used by the WHO as the standard for recording obesity statistics since the early 1980s.
This general correlation is particularly useful for consensus data regarding obesity or various other conditions because it can be used to build a semi-accurate representation from which a solution can be stipulated, or the RDA for a group can be calculated. Similarly, this is becoming more and more pertinent to the growth of children, since the majority of children are sedentary. Cross-sectional studies indicated that sedentary people can decrease BMI by becoming more physically active. Smaller effects are seen in prospective cohort studies which lend to support active mobility as a means to prevent a further increase in BMI.
Legislation
In France, Italy, and Spain, legislation has been introduced banning the usage of fashion show models having a BMI below 18. In Israel, a model with BMI below 18.5 is banned. This is done to fight anorexia among models and people interested in fashion.
Relationship to health
A study published by Journal of the American Medical Association (JAMA) in 2005 showed that overweight people had a death rate similar to normal weight people as defined by BMI, while underweight and obese people had a higher death rate.
A study published by The Lancet in 2009 involving 900,000 adults showed that overweight and underweight people both had a mortality rate higher than normal weight people as defined by BMI. The optimal BMI was found to be in the range of 22.5–25. The average BMI of athletes is 22.4 for women and 23.6 for men.
High BMI is associated with type 2 diabetes only in people with high serum gamma-glutamyl transpeptidase.
In an analysis of 40 studies involving 250,000 people, patients with coronary artery disease with normal BMIs were at higher risk of death from cardiovascular disease than people whose BMIs put them in the overweight range (BMI 25–29.9).
One study found that BMI had a good general correlation with body fat percentage, and noted that obesity has overtaken smoking as the world's number one cause of death. But it also notes that in the study 50% of men and 62% of women were obese according to body fat defined obesity, while only 21% of men and 31% of women were obese according to BMI, meaning that BMI was found to underestimate the number of obese subjects.
A 2010 study that followed 11,000 subjects for up to eight years concluded that BMI is not the most appropriate measure for the risk of heart attack, stroke or death. A better measure was found to be the waist-to-height ratio. A 2011 study that followed 60,000 participants for up to 13 years found that waist–hip ratio was a better predictor of ischaemic heart disease mortality.
Limitations

The medical establishment and statistical community have both highlighted the limitations of BMI.
Racial and gender differences
Part of the statistical limitations of the BMI scale is the result of Quetelet's original sampling methods. As noted in his primary work, A Treatise on Man and the Development of His Faculties, the data from which Quetelet derived his formula was taken mostly from Scottish Highland soldiers and French Gendarmerie. The BMI was always designed as a metric for European men. For women, and people of non-European origin, the scale is often biased. As noted by sociologist Sabrina Strings, the BMI is largely inaccurate for black people especially, disproportionately labelling them as overweight even for healthy individuals.
Scaling
The exponent in the denominator of the formula for BMI is arbitrary. The BMI depends upon weight and the square of height. Since mass increases to the third power of linear dimensions, taller individuals with exactly the same body shape and relative composition have a larger BMI. BMI is proportional to the mass and inversely proportional to the square of the height. So, if all body dimensions double, and mass scales naturally with the cube of the height, then BMI doubles instead of remaining the same. This results in taller people having a reported BMI that is uncharacteristically high, compared to their actual body fat levels. In comparison, the Ponderal index is based on the natural scaling of mass with the third power of the height.
However, many taller people are not just "scaled up" short people but tend to have narrower frames in proportion to their height. Carl Lavie has written that "The B.M.I. tables are excellent for identifying obesity and body fat in large populations, but they are far less reliable for determining fatness in individuals."
For US adults, exponent estimates range from 1.92 to 1.96 for males and from 1.45 to 1.95 for females.
Physical characteristics
The BMI overestimates roughly 10% for a large (or tall) frame and underestimates roughly 10% for a smaller frame (short stature). In other words, people with small frames would be carrying more fat than optimal, but their BMI indicates that they are normal. Conversely, large framed (or tall) individuals may be quite healthy, with a fairly low body fat percentage, but be classified as overweight by BMI.
For example, a height/weight chart may say the ideal weight (BMI 21.5) for a 1.78-metre-tall (5 ft 10 in) man is 68 kilograms (150 lb). But if that man has a slender build (small frame), he may be overweight at 68 kg or 150 lb and should reduce by 10% to roughly 61 kg or 135 lb (BMI 19.4). In the reverse, the man with a larger frame and more solid build should increase by 10%, to roughly 75 kg or 165 lb (BMI 23.7). If one teeters on the edge of small/medium or medium/large, common sense should be used in calculating one's ideal weight. However, falling into one's ideal weight range for height and build is still not as accurate in determining health risk factors as waist-to-height ratio and actual body fat percentage.
Accurate frame size calculators use several measurements (wrist circumference, elbow width, neck circumference, and others) to determine what category an individual falls into for a given height. The BMI also fails to take into account loss of height through ageing. In this situation, BMI will increase without any corresponding increase in weight.
Muscle versus fat
Assumptions about the distribution between muscle mass and fat mass are inexact. BMI generally overestimates adiposity on those with leaner body mass (e.g., athletes) and underestimates excess adiposity on those with fattier body mass.
A study in June 2008 by Romero-Corral et al. examined 13,601 subjects from the United States' third National Health and Nutrition Examination Survey (NHANES III) and found that BMI-defined obesity (BMI ≥ 30) was present in 21% of men and 31% of women. Body fat-defined obesity was found in 50% of men and 62% of women. While BMI-defined obesity showed high specificity (95% for men and 99% for women), BMI showed poor sensitivity (36% for men and 49% for women). In other words, the BMI will be mostly correct when determining a person to be obese, but can err quite frequently when determining a person not to be. Despite this undercounting of obesity by BMI, BMI values in the intermediate BMI range of 20–30 were found to be associated with a wide range of body fat percentages. For men with a BMI of 25, about 20% have a body fat percentage below 20% and about 10% have body fat percentage above 30%.
Body composition for athletes is often better calculated using measures of body fat, as determined by such techniques as skinfold measurements or underwater weighing and the limitations of manual measurement have also led to new, alternative methods to measure obesity, such as the body volume indicator.
Variation in definitions of categories
It is not clear where on the BMI scale the threshold for overweight and obese should be set. Because of this, the standards have varied over the past few decades. Between 1980 and 2000 the U.S. Dietary Guidelines have defined overweight at a variety of levels ranging from a BMI of 24.9 to 27.1. In 1985 the National Institutes of Health (NIH) consensus conference recommended that overweight BMI be set at a BMI of 27.8 for men and 27.3 for women.
In 1998, an NIH report concluded that a BMI over 25 is overweight and a BMI over 30 is obese. In the 1990s the World Health Organization (WHO) decided that a BMI of 25 to 30 should be considered overweight and a BMI over 30 is obese, the standards the NIH set. This became the definitive guide for determining if someone is overweight.
One study found that the vast majority of people labelled 'overweight' and 'obese' according to current definitions do not in fact face any meaningful increased risk for early death. In a quantitative analysis of several studies, involving more than 600,000 men and women, the lowest mortality rates were found for people with BMIs between 23 and 29; most of the 25–30 range considered 'overweight' was not associated with higher risk.
Alternatives
Corpulence index (exponent of 3)
The corpulence index uses an exponent of 3 rather than 2. The corpulence index yields valid results even for very short and very tall people, which is a problem with BMI. For example, a 152.4 cm (5 ft 0 in) tall person at an ideal body weight of 48 kg (106 lb) gives a normal BMI of 20.74 and CI of 13.6, while a 200 cm (6 ft 7 in) tall person with a weight of 100 kg (220 lb) gives a BMI of 24.84, very close to an overweight BMI of 25, and a CI of 12.4, very close to a normal CI of 12.
New BMI (exponent of 2.5)
An exponent of 5/2 was proposed by Quetelet in the 19th century:
In general, we do not err much when we assume that during development the squares of the weight at different ages are as the fifth powers of the height
This exponent of 2.5 is used in a revised formula for Body Mass Index, proposed by Nick Trefethen, Professor of numerical analysis at the University of Oxford, which minimizes the distortions for shorter and taller individuals resulting from the use of an exponent of 2 in the traditional BMI formula:
The scaling factor of 1.3 was determined to make the proposed new BMI formula align with the traditional BMI formula for adults of average height, while the exponent of 2.5 is a compromise between the exponent of 2 in the traditional formula for BMI and the exponent of 3 that would be expected for the scaling of weight (which at constant density would theoretically scale with volume, i.e., as the cube of the height) with height. In Trefethen's analysis, an exponent of 2.5 was found to fit empirical data more closely with less distortion than either an exponent of 2 or 3.
BMI prime (exponent of 2, normalization factor)
BMI Prime, a modification of the BMI system, is the ratio of actual BMI to upper limit optimal BMI (currently defined at 25 kg/m2), i.e., the actual BMI expressed as a proportion of upper limit optimal. BMI Prime is a dimensionless number independent of units. Individuals with BMI Prime less than 0.74 are underweight; those with between 0.74 and 1.00 have optimal weight; and those at 1.00 or greater are overweight. BMI Prime is useful clinically because it shows by what ratio (e.g. 1.36) or percentage (e.g. 136%, or 36% above) a person deviates from the maximum optimal BMI.
For instance, a person with BMI 34 kg/m2 has a BMI Prime of 34/25 = 1.36, and is 36% over their upper mass limit. In South East Asian and South Chinese populations (see § international variations), BMI Prime should be calculated using an upper limit BMI of 23 in the denominator instead of 25. BMI Prime allows easy comparison between populations whose upper-limit optimal BMI values differ.
Waist circumference
Waist circumference is a good indicator of visceral fat, which poses more health risks than fat elsewhere. According to the U.S. National Institutes of Health (NIH), waist circumference in excess of 1,020 mm (40 in) for men and 880 mm (35 in) for (non-pregnant) women is considered to imply a high risk for type 2 diabetes, dyslipidemia, hypertension, and cardiovascular disease CVD. Waist circumference can be a better indicator of obesity-related disease risk than BMI. For example, this is the case in populations of Asian descent and older people. 940 mm (37 in) for men and 800 mm (31 in) for women has been stated to pose "higher risk", with the NIH figures "even higher".
Waist-to-hip circumference ratio has also been used, but has been found to be no better than waist circumference alone, and more complicated to measure.
A related indicator is waist circumference divided by height. The values indicating increased risk are: greater than 0.5 for people under 40 years of age, 0.5 to 0.6 for people aged 40–50, and greater than 0.6 for people over 50 years of age.
Surface-based body shape index
The Surface-based Body Shape Index (SBSI) is far more rigorous and is based upon four key measurements: the body surface area (BSA), vertical trunk circumference (VTC), waist circumference (WC) and height (H). Data on 11,808 subjects from the National Health and Human Nutrition Examination Surveys (NHANES) 1999–2004, showed that SBSI outperformed BMI, waist circumference, and A Body Shape Index (ABSI), an alternative to BMI.
A simplified, dimensionless form of SBSI, known as SBSI*, has also been developed.
Modified body mass index
Within some medical contexts, such as familial amyloid polyneuropathy, serum albumin is factored in to produce a modified body mass index (mBMI). The mBMI can be obtained by multiplying the BMI by serum albumin, in grams per litre.
See also
- Allometry
- Body water
- History of anthropometry
- List of countries by body mass index
- Obesity paradox
- Relative Fat Mass
- Somatotype and constitutional psychology
Further reading
- Ferrera LA, ed. (2006). Focus on Body Mass Index And Health Research. New York: Nova Science. ISBN 978-1-59454-963-2.
- Samaras TT, ed. (2007). Human Body Size and the Laws of Scaling: Physiological, Performance, Growth, Longevity and Ecological Ramifications. New York: Nova Science. ISBN 978-1-60021-408-0.
- Sothern MS, Gordon ST, von Almen TK, eds. (19 April 2016). Handbook of Pediatric Obesity: Clinical Management (Illustrated ed.). CRC Press. ISBN 978-1-4200-1911-7.
External links
- U.S. National Center for Health Statistics:
- "BMI Growth Charts for children and young adults". US Centers for Disease Control and Prevention. 31 January 2019.
- "BMI calculator ages 20 and older". US Centers for Disease Control and Prevention. 21 July 2021.
| この記事は、クリエイティブ・コモンズ・表示・継承ライセンス3.0のもとで公表されたウィキペディアの項目Body mass index(26 February 2024編集記事参照)を素材として二次利用しています。 Item:Q21276 |